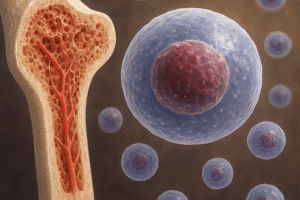
Bone healing is a complex biological process influenced by an interplay of cellular activities, signaling molecules, and the **genetic** blueprint unique to each individual. Understanding how genetic factors shape the pace and efficiency of bone repair has profound implications for improving patient outcomes in orthopedics and regenerative medicine. This article explores the key genetic determinants of bone regeneration, the molecular pathways they govern, and emerging clinical strategies that harness genetic insights for enhanced recovery.
Role of Genetic Variation in Bone Regeneration
Inter-individual differences in bone healing rates often trace back to **polymorphisms**—variations in DNA sequence that can affect gene function and expression. These genetic variants may modulate the activity of critical proteins involved in **osteogenesis**, the process of new bone formation, or influence the recruitment and differentiation of repair cells at the injury site.
Genetic Polymorphisms and Healing Outcomes
- SNPs in the COL1A1 gene can alter **collagen** synthesis, affecting bone matrix quality.
- Variants of the VDR (vitamin D receptor) gene may influence calcium absorption and mineralization rates.
- Mutations in the IL-6 promoter region can modulate levels of inflammatory **cytokines**, impacting the early healing phase.
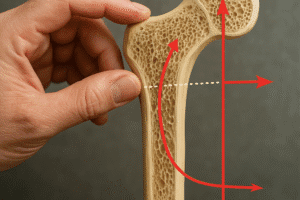
Gene Expression Profiles During Repair
Advanced transcriptomic analyses reveal distinct patterns of gene activation in individuals with rapid versus delayed bone healing. In fast healers:
- Upregulation of BMPs (bone morphogenetic proteins) accelerates osteoblast differentiation.
- Elevated RUNX2 expression ensures robust commitment of progenitor cells to the bone lineage.
- Balanced MMP (matrix metalloproteinases) activity fine-tunes extracellular matrix remodeling.
Conversely, delayed repair often associates with prolonged expression of osteoclast-related genes, hinting at an imbalance between bone formation and resorption.
Molecular Pathways Controlled by Genetic Factors
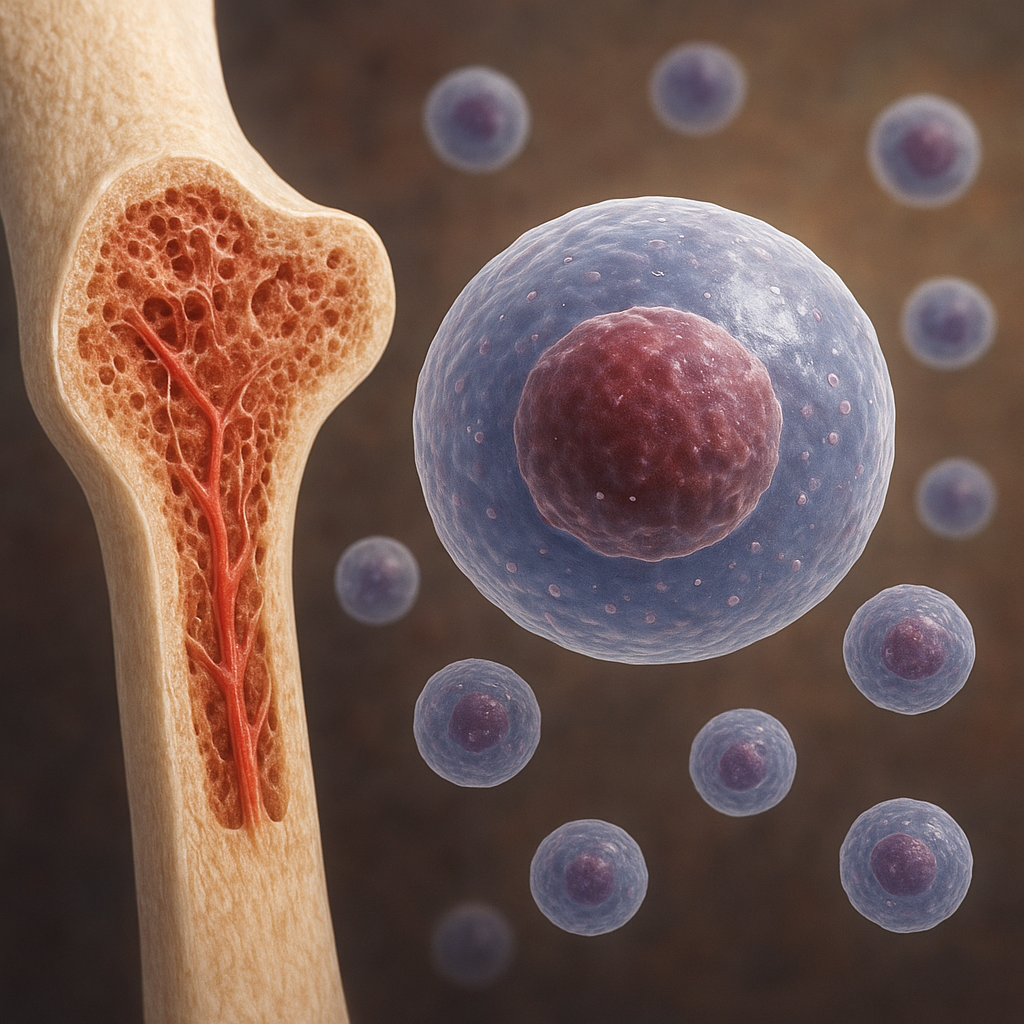
The orchestration of bone repair relies on tightly regulated signaling cascades. Key genetic entities coordinate these molecular events, directing the behavior of **osteoblast** and **osteoclast** populations, as well as shaping the local **microenvironment** for optimal regeneration.
Growth Factors and Cytokine Networks
Genetic regulation of growth factors determines the intensity and duration of signals that drive cell proliferation and differentiation:
- BMPs family members, encoded by BMP2 and BMP7 genes, activate SMAD pathways crucial for early bone formation.
- TGF-β signaling, influenced by TGFB1 gene variants, modulates extracellular matrix deposition and immune cell recruitment.
- Genetic control of VEGF (vascular endothelial growth factor) expression affects angiogenesis, ensuring nutrient delivery and waste removal.
Transcription Factors and Epigenetic Modifiers
At the genomic level, transcription factors interpret genetic codes to launch repair programs:
- RUNX2, often termed the “master regulator” of osteoblastogenesis, is essential for early lineage commitment.
- SP7 (Osterix) downstream of RUNX2 ensures maturation of osteoblasts capable of producing **collagen**-rich matrix.
- Epigenetic regulators such as HDACs and DNMTs, influenced by genetic variants, shape chromatin accessibility and gene expression kinetics.
Furthermore, non-coding RNAs—including microRNAs encoded within genetic loci—fine-tune post-transcriptional control, ensuring that pro-healing factors are synthesized at the right time and quantity.
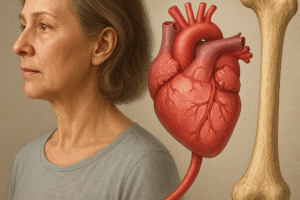
Clinical Implications and Therapeutic Strategies
Translating genetic insights into clinical practice paves the way for **personalized** approaches that optimize bone repair for individual patients. From preoperative screening to gene-based therapies, the era of precision orthopedics is emerging.
Genetic Screening and Risk Stratification
- Preoperative genotyping for key variants (e.g., COL1A1, VDR, TGFB1) can identify patients at risk for delayed healing or nonunion.
- Customized rehabilitation protocols, including weight-bearing schedules and nutritional support, may be tailored based on genetic risk profiles.
- Pharmacogenomic data help predict individual responses to bone anabolic agents like PTH analogs or bisphosphonates.
Gene Therapy and Advanced Treatments
Emerging interventions aim to correct or enhance genetic signals directly at the injury site:
- Local delivery of viral vectors carrying BMP2 or RUNX2 transgenes stimulates robust **osteogenesis** in challenging fractures.
- CRISPR-based gene editing holds promise for repairing deleterious mutations in collagen genes, restoring normal matrix formation.
- Stem cell therapies combined with gene-modified scaffolds can create a favorable **microenvironment** that balances osteoblast and osteoclast activity.
Nanoparticle carriers and hydrogel systems further refine the spatial and temporal release of therapeutic genes, minimizing off-target effects and immune responses.
Future Directions in Genetic Research for Bone Healing
Ongoing studies leveraging genome-wide association studies (GWAS) and single-cell sequencing promise to uncover novel genetic determinants of bone repair. Integrating multi-omics data—genomics, transcriptomics, proteomics—and applying machine learning algorithms will build predictive models of healing trajectories. Ultimately, a comprehensive genetic atlas of bone regeneration could revolutionize how clinicians forecast, monitor, and enhance fracture recovery for each patient.