The intricate landscape of bone tissue extends far beyond its visible anatomy, reaching into the realm of microarchitecture where cellular activities and mineral deposition define strength, flexibility, and resilience. Understanding this delicate network reveals how bones adapt to mechanical demands, respond to metabolic changes, and succumb to disease. Insights into bone microarchitecture inform diagnosis, guide treatment strategies, and inspire novel approaches in tissue engineering. This article explores structural features of trabecular and cortical regions, surveys advanced imaging modalities, examines clinical applications, and highlights emerging trends in bone science.
Bone Microarchitecture: Structure and Function
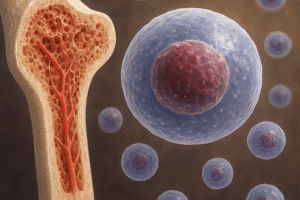
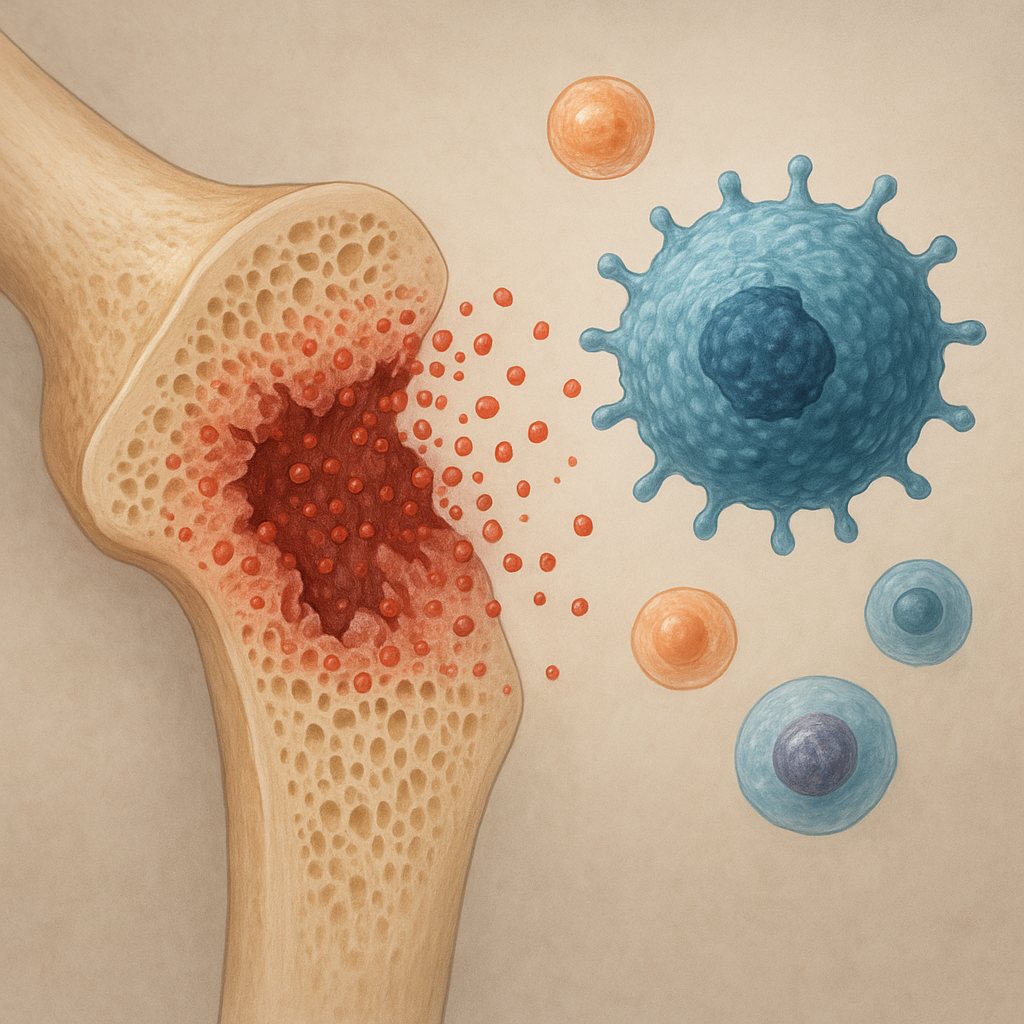
Bone tissue comprises two primary structural compartments: the porous, honeycomb-like trabecular network and the dense, protective cortical shell. The interplay of these compartments imparts both stiffness and energy absorption capabilities. Microstructural parameters such as trabecular thickness, separation, and connectivity, along with cortical porosity and thickness, dictate overall skeletal integrity. At a molecular level, collagen fibrils provide a flexible matrix while hydroxyapatite crystals ensure mineralization. Continuous bone remodeling, orchestrated by osteoblasts and osteoclasts, maintains homeostasis in response to mechanical loading and systemic cues.
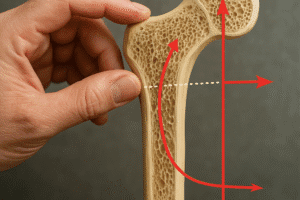
Trabecular Bone Architecture
Trabecular bone resides mainly in vertebral bodies, metaphyses of long bones, and the pelvis. Its lattice-like structure maximizes strength-to-weight ratio, enabling rapid adaptation to stress via remodeling. Key parameters include:
- Trabecular thickness: Average diameter of rods or plates.
- Trabecular separation: Distance between trabeculae, influencing stiffness.
- Structural model index (SMI): Characterizes rod-like versus plate-like geometry.
- Connectivity density: Number of connections per unit volume.
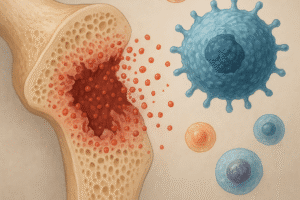
Alterations in these metrics underlie conditions such as osteoporosis, where loss of connectivity greatly elevates fracture risk, especially in the spine and hip.
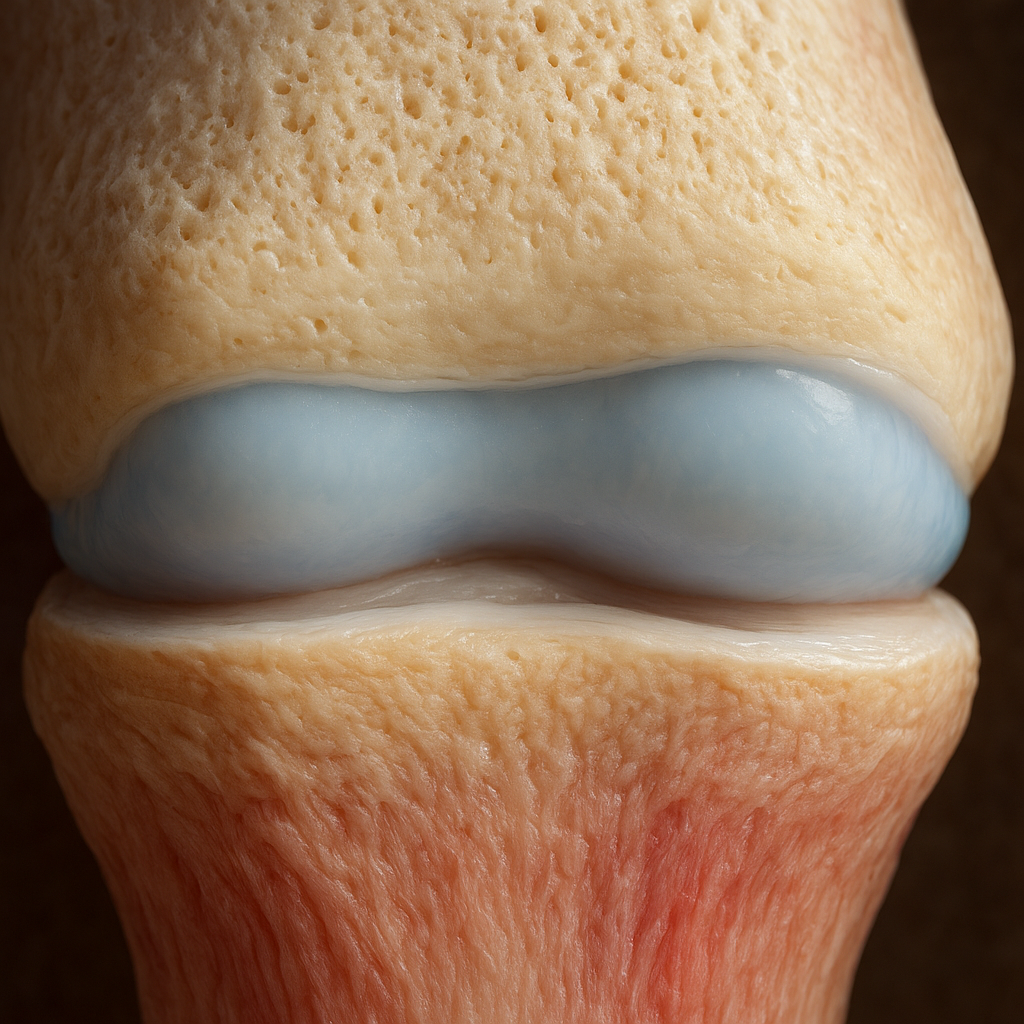
Cortical Bone Characteristics
Cortical bone forms the outer shell of most skeletal elements, providing load-bearing capacity and protection of marrow spaces. Mechanical competence depends on cortical thickness, porosity, and microcrack density. Age-related increases in intracortical porosity weaken bone by reducing effective cross-sectional area and creating stress risers. Low-intensity loading can lead to microdamage accumulation, while regular mechanical stimuli promote modeling responses that thicken the cortex.
Techniques for Assessing Bone Microarchitecture
Assessing microstructural details is critical for research and clinical evaluation. Conventional X-ray densitometry measures areal bone mineral density but lack spatial resolution. Advanced modalities offer volumetric insights and quantifiable metrics.
Micro-Computed Tomography (micro-CT)
micro-CT provides high-resolution, three-dimensional images of ex vivo bone specimens. Typical voxel sizes range from 1 to 10 µm, enabling direct measurement of trabecular and cortical parameters. Advantages include non-destructive analysis, isotropic resolution, and compatibility with mechanical testing setups. Limitations involve radiation dose, scan time, and restricted use to small samples. In research, micro-CT is the gold standard for preclinical studies of bone quality.
High-Resolution Peripheral Quantitative Computed Tomography (HR-pQCT)
HR-pQCT extends micro-CT principles to in vivo assessments at peripheral sites like the distal radius and tibia. With voxel sizes near 60 µm, it quantifies trabecular thickness, separation, and cortical porosity. Studies demonstrate its value in predicting fracture risk beyond dual-energy X-ray absorptiometry. However, motion artifacts and limited skeletal sites pose challenges.
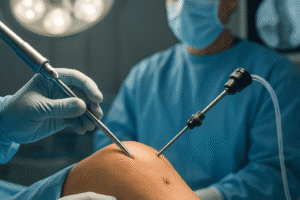
Histomorphometry
Bone histomorphometry involves microscopic analysis of stained biopsy sections, yielding dynamic and static indices of bone formation, resorption, and structure. Tetracycline labels administered pre-biopsy reveal mineralizing surfaces, providing turnover rates. Although invasive, histomorphometry remains a definitive method for evaluating cellular activity and the effects of therapeutic agents on remodeling.
Magnetic Resonance Imaging (MRI)
Advances in MRI technology permit visualization of bone microarchitecture without ionizing radiation. Ultrashort echo time (UTE) sequences capture bone signal intensity, while high-field systems improve spatial resolution. MRI metrics correlate with mechanical properties, but accessibility and cost limit widespread application.
Clinical Implications and Applications
Elucidating bone microarchitecture advances diagnosis, treatment planning, and monitoring of skeletal disorders. Quantitative metrics inform fracture risk assessment, personalized therapies, and implant design.
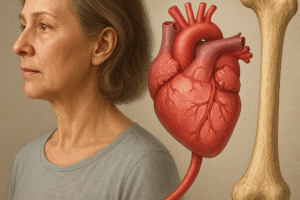
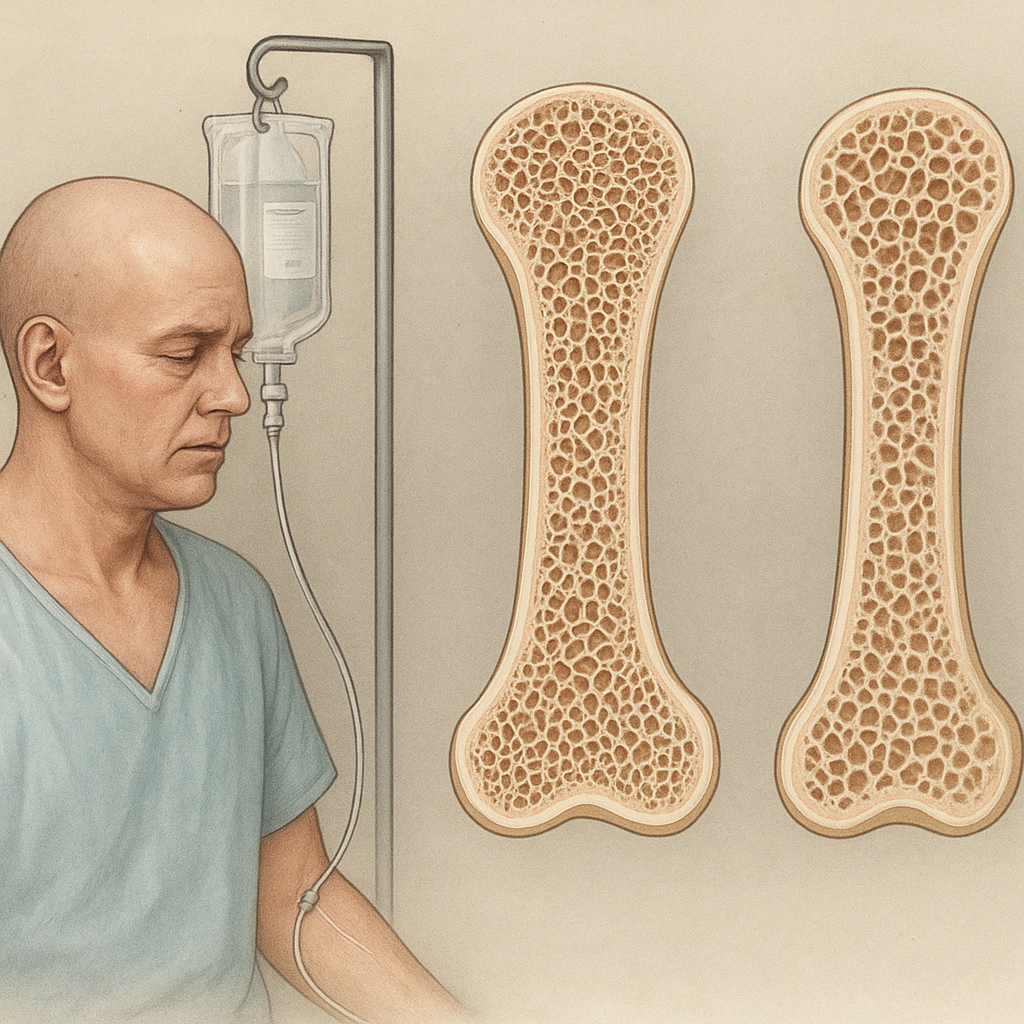
Osteoporosis and Fracture Risk
While osteoporosis is traditionally defined by low bone mineral density, microarchitectural deterioration significantly contributes to fragility. HR-pQCT studies reveal that cortical thinning and trabecular perforation predict fractures in postmenopausal women, even when densitometry values are borderline. Incorporating microstructural analysis into clinical routines could refine risk stratification and guide interventions such as antiresorptive or anabolic agents.
Biomechanics of Implants and Scaffolds
Successful orthopedic and dental implants require integration with host bone at the micro- and nano-scale. Understanding the biomechanics of peri-implant bone, including load transfer and stress distribution, informs design of surface textures and porous scaffolds that mimic natural microarchitecture. Finite element modeling allows simulation of implant-bone interactions, predicting regions susceptible to stress shielding or overload.
Bone Regeneration and Tissue Engineering
Tissue engineering strategies aim to recreate hierarchical bone structures. Biomaterial scaffolds with controlled pore size, interconnectivity, and bioactive coatings support osteointegration and vascularization. Combining osteogenic cells, growth factors, and dynamic bioreactors yields constructs with optimized remodeling potential. Cutting-edge approaches leverage 3D bioprinting and regeneration factors to fabricate patient-specific grafts that restore both form and function.
Advances and Future Directions
Emerging technologies promise to deepen our understanding of bone microarchitecture and accelerate translation into clinical practice. Machine learning algorithms applied to imaging datasets can identify subtle microstructural patterns predictive of disease progression. Finite element analysis, integrated with patient-specific models, will enable personalized load simulations and optimized therapeutic plans. Nanotechnology and bioinspired mineralization processes are poised to enhance scaffold performance and stimulate natural bone healing. Ultimately, a multidisciplinary approach uniting biomechanics, materials science, and cellular biology will drive innovations that preserve skeletal health throughout life.