Alcohol intake has profound consequences on the skeletal system, influencing both bone development and maintenance. This article explores the biochemical pathways affected by ethanol, the clinical outcomes of prolonged consumption, and potential strategies to counteract its negative effects. Through examining molecular mechanisms, risk factors, and therapeutic interventions, we aim to provide a comprehensive understanding of how alcohol alters bone physiology.
Molecular Mechanisms of Alcohol-Induced Bone Deterioration
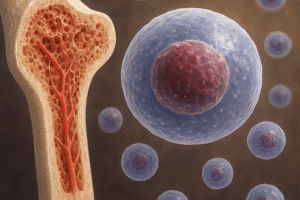
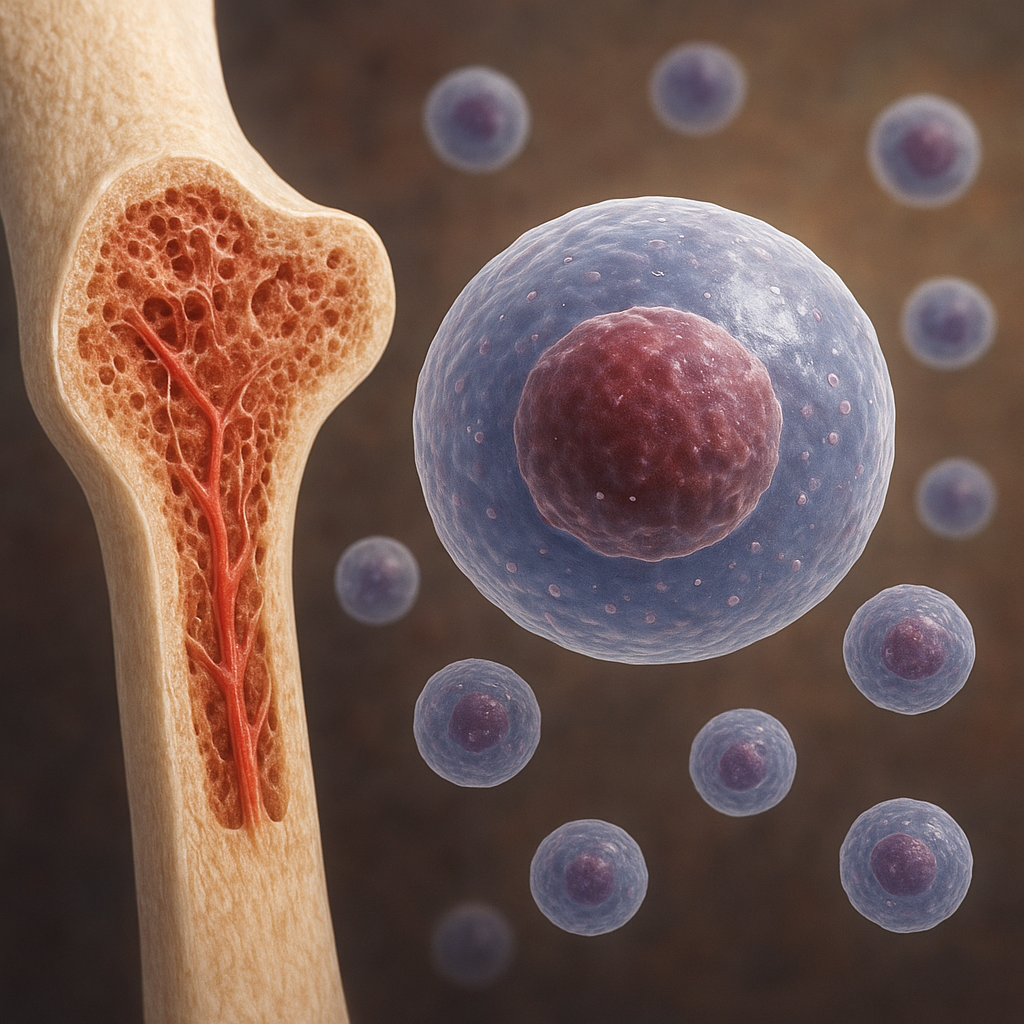
Impact on Osteoblast Function
Osteoblasts are specialized cells responsible for synthesizing new bone matrix and facilitating mineral deposition. Chronic alcohol exposure disrupts the proliferation and differentiation of these cells, leading to impaired formation of bone tissue. Ethanol metabolites, including acetaldehyde, can interfere with signaling pathways such as Wnt/β-catenin and inhibit transcription factors critical for osteoblastogenesis. Additionally, alcohol downregulates the production of osteocalcin and reduces expression of alkaline phosphatase, key markers of active bone formation.
Oxidative Stress and Inflammation
Excessive alcohol consumption generates reactive oxygen species (ROS) that overwhelm the antioxidant defenses of bone microenvironment. This oxidative stress leads to lipid peroxidation, DNA damage, and protein oxidation in bone cells. Furthermore, alcohol upregulates pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6), fostering a catabolic milieu. Chronic inflammation accelerates bone resorption by stimulating osteoclast activity while simultaneously inhibiting osteoblast function, thus skewing the remodeling balance toward net bone loss.
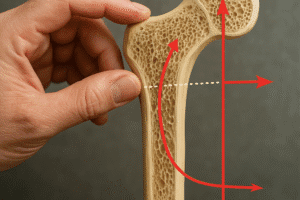
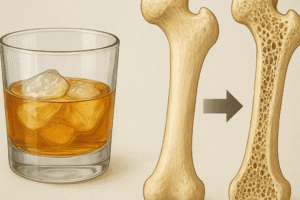
Disruption of Calcium Homeostasis
Maintaining optimal bone mineralization depends on precise regulation of calcium and phosphate levels. Alcohol interferes with gastrointestinal absorption of calcium, impairs vitamin D metabolism in the liver and kidneys, and enhances urinary excretion of minerals. Consequently, serum calcium fluctuations trigger secondary hyperparathyroidism, increasing parathyroid hormone (PTH) secretion and activating osteoclast-mediated bone resorption. Over time, this dysregulation contributes to diminished bone mineral density and compromised structural integrity.
Clinical Implications and Risk Factors
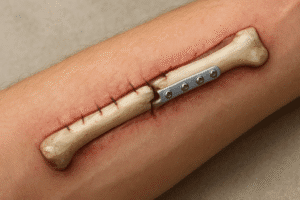
Osteoporosis and Fracture Healing
Individuals with a history of heavy alcohol use exhibit a higher prevalence of osteoporosis, characterized by porous and fragile bones. Reduced bone strength significantly raises the risk of fractures in multiple anatomical sites, including the hip, spine, and wrist. Moreover, alcohol impairs the normal healing process by altering callus formation and delaying mineralization at fracture sites. Clinically, patients often present with non-union or delayed-union fractures, necessitating extended immobilization and rehabilitation protocols.
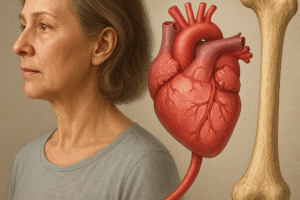
Age, Gender, and Genetic Predisposition
While alcohol exerts detrimental effects across all demographics, certain populations are particularly susceptible. Postmenopausal women lose the protective influence of estrogen on bone, amplifying alcohol’s catabolic impact on skeletal tissue. Similarly, older adults experience age-related declines in bone turnover, compounding alcohol-induced inhibition of osteogenesis. Genetic variations in alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) enzymes also modulate individual vulnerability by altering the rate of ethanol metabolism and accumulation of toxic intermediates.
Comorbid Conditions and Nutritional Status
Alcohol use disorder often coexists with malnutrition, liver disease, and hormonal imbalances that further compromise bone health. Deficiencies in protein, vitamins K and C, and trace elements such as magnesium and zinc hinder collagen synthesis and cross-linking. Liver cirrhosis impairs activation of vitamin D and disrupts estrogen metabolism, exacerbating bone loss. Understanding these interrelated factors is essential for comprehensive risk assessment and personalized management strategies.
Preventive Strategies and Therapeutic Interventions
Dietary and Lifestyle Modifications
Adopting a balanced diet rich in calcium, vitamin D, and protein is fundamental for mitigating alcohol’s impact on bone. Foods such as dairy products, leafy greens, and fortified cereals support mineral intake, while sunlight exposure enhances endogenous vitamin D synthesis. Regular weight-bearing exercise stimulates osteogenic pathways and improves bone strength. Cessation or reduction of alcohol consumption remains the most effective approach to halt further bone deterioration and allow partial recovery of skeletal function.
- Limit daily alcohol to recommended guidelines
- Engage in resistance training and aerobic activities
- Ensure adequate intake of micronutrients
- Monitor bone density periodically
Pharmacological Approaches
When lifestyle changes are insufficient, pharmacotherapy can play a key role in preserving bone mass. Bisphosphonates inhibit osteoclast-mediated resorption, whereas selective estrogen receptor modulators (SERMs) mimic estrogen’s protective effects on bone. Denosumab, a monoclonal antibody targeting RANKL, offers another option to reduce bone turnover. In patients with severe deficiency, calcitriol or cholecalciferol supplementation corrects hypovitaminosis D. Tailoring treatment requires careful evaluation of comorbidities, medication interactions, and fracture risk assessment tools.
Emerging Research Directions
Novel strategies aim to counteract alcohol-induced bone damage at the molecular level. Antioxidant therapies, including N-acetylcysteine and resveratrol, have shown promise in preclinical studies by scavenging ROS and modulating inflammatory pathways. Gene therapy approaches targeting growth factors such as bone morphogenetic proteins (BMPs) seek to enhance osteogenic differentiation. Additionally, research into the gut–bone axis explores how alcohol-altered microbiota influence systemic inflammation and nutrient absorption. These innovative lines of inquiry may yield next-generation therapeutics to restore skeletal health.
Conclusion of Current Insights
Decades of research underscore the multifaceted mechanisms by which alcohol undermines bone integrity, from cellular toxicity to systemic metabolic disruption. Recognizing the interplay of risk factors and implementing targeted interventions can substantially mitigate long-term skeletal consequences. Future advancements in pharmacology, nutrition science, and personalized medicine hold the potential to revolutionize care for individuals affected by alcohol-related bone disease.