Osteogenesis Imperfecta is a complex disorder affecting the skeletal framework, often referred to as brittle bone disease. This condition arises from defects in the body’s ability to produce normal collagen, resulting in fragile bones, frequent fractures, and a range of extra-skeletal manifestations. Understanding its underlying mechanisms, approaches to diagnosis, and comprehensive management strategies is essential for improving patient outcomes and enhancing quality of life.
Etiology and Pathophysiology
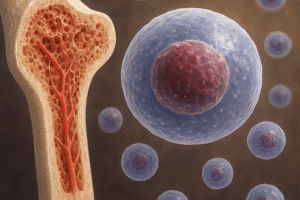
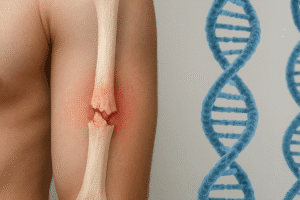
At the heart of Osteogenesis Imperfecta lies a genetic mutation affecting the genes responsible for type I collagen production, primarily COL1A1 and COL1A2. Collagen type I is a primary component of bone matrix, providing tensile strength and structural support. When mutations disrupt the normal assembly of collagen fibers, the resulting bone matrix is weak, leading to reduced bone density and increased susceptibility to microfractures and complete breaks.
Genetic Basis
- Autosomal Dominant Mutations: The majority of cases are inherited in an autosomal dominant fashion, where a single copy of the defective gene suffices to cause the disorder.
- Autosomal Recessive Forms: Less common variants arise from autosomal recessive inheritance, often involving genes related to collagen post-translational modification.
- De Novo Mutations: In some individuals, new spontaneous mutations occur without a family history, emphasizing the importance of genetic counseling.
Molecular Mechanisms
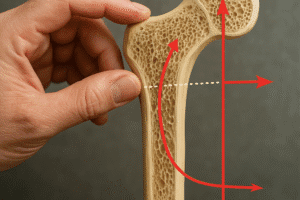
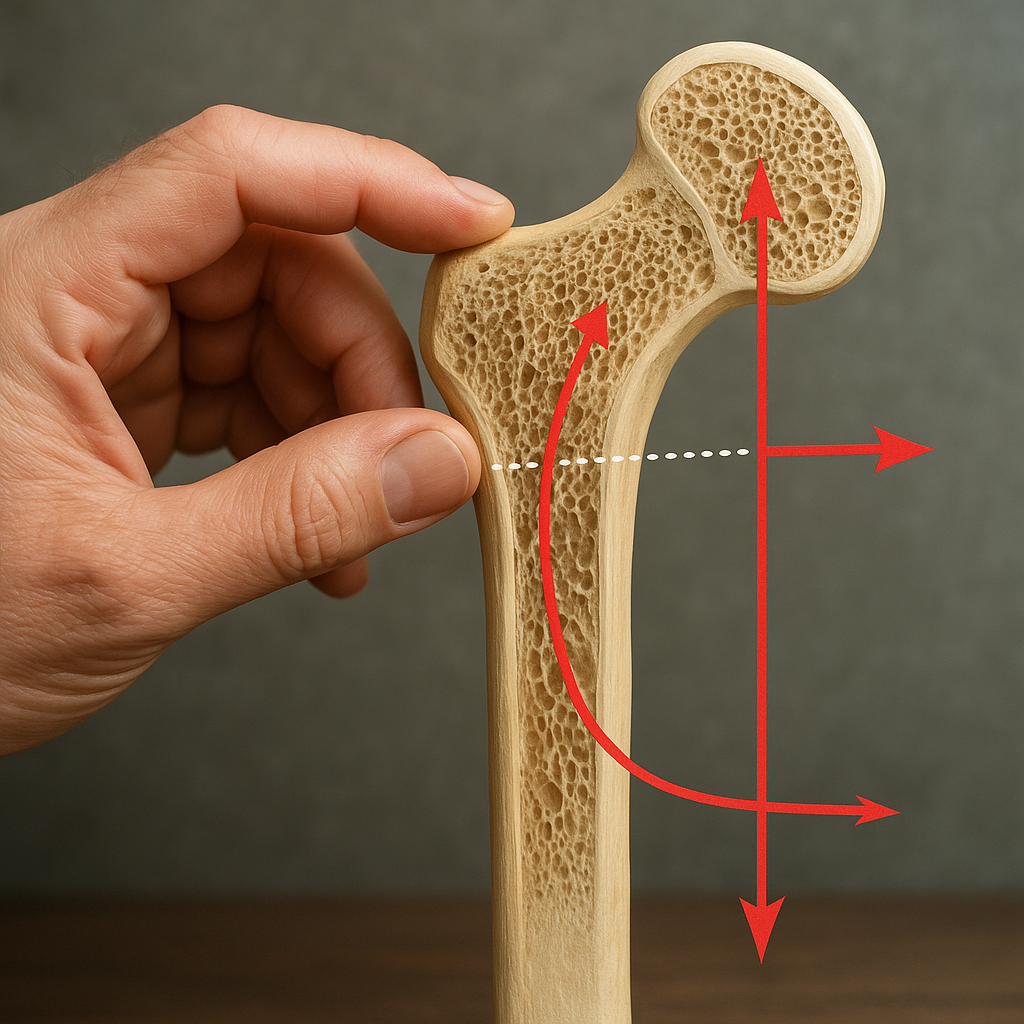
Defective collagen molecules can lead to improper fibril formation, altering the mineralization process that usually confers hardness to bone tissue. The result is a porous, thin cortical shell around the bone, leading to frequent microdamages that accumulate into larger fractures. Additionally, alterations in collagen affect tendon strength and joint stability, contributing to joint laxity and muscle weakness.
Clinical Presentation and Diagnosis
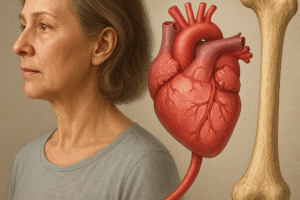
Osteogenesis Imperfecta exhibits a broad clinical spectrum, from mild forms with few fractures to severe, perinatal-lethal types. Recognizing hallmark signs and conducting timely investigations can dramatically influence treatment planning and prognosis.
Key Clinical Features
- Bone Fragility: Recurrent fractures following minimal trauma are the most prominent symptom.
- Blue Sclerae: Thinning of the collagen-rich sclera allows underlying choroidal veins to show through, creating a characteristic blue hue.
- Dentinogenesis Imperfecta: Abnormal tooth development leading to discolored, translucent teeth susceptible to wear.
- Hearing Loss: Conductive or sensorineural hearing impairment arises in adolescence or early adulthood.
- Short Stature and Skeletal Deformities: Bowing of long bones, vertebral compression, and scoliosis may be evident.
Diagnostic Workup
Early and accurate diagnosis relies on a combination of clinical evaluation, imaging studies, and genetic testing:
- Radiographic Assessment: X-rays reveal cortical thinning, bone deformities, and evidence of healing fractures.
- Bone Densitometry (DEXA): Quantifies bone density to assess severity and monitor progression.
- Biochemical Markers: Serum levels of collagen breakdown products and bone turnover markers offer insight into remodeling rates.
- Genetic Analysis: Sequencing COL1A1, COL1A2, and related genes confirms specific mutations, guiding prognosis and family planning.
Management and Treatment Strategies
Managing Osteogenesis Imperfecta requires a multidisciplinary approach, aiming to reduce fracture risk, optimize mobility, and address extra-skeletal complications. Interventions span pharmacologic, surgical, and rehabilitative domains.
Pharmacologic Interventions
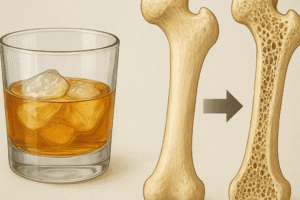
- Bisphosphonates: These agents inhibit osteoclast-mediated bone resorption, leading to increased bone density and reduced fracture rates. Intravenous pamidronate and zoledronic acid are commonly used.
- Denosumab: A monoclonal antibody targeting RANKL, it offers an alternative for patients intolerant to bisphosphonates.
- Teriparatide: Intermittent parathyroid hormone analog promotes bone formation and has been explored in adult OI cases.
- Vitamin D and Calcium Supplementation: Essential cofactors for mineralization and general bone health.
Orthopedic and Surgical Approaches
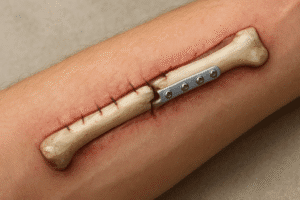
- Rodding Procedures: Insertion of intramedullary rods into long bones to prevent deformities and support structural integrity.
- Spinal Fusion: Stabilization for severe scoliosis to improve posture and reduce pain.
- Fracture Management: Gentle casting, splinting, or surgical fixation depending on fracture location and patient age.
Rehabilitation and Supportive Care
Physical therapy and physiotherapy play a pivotal role in strengthening muscles, improving balance, and preventing contractures. A tailored exercise program emphasizes low-impact activities such as swimming and cycling to minimize risk. Occupational therapy assists in adapting daily activities and home environments for safety. Use of orthotic devices, braces, and mobility aids enhances independence and reduces fall risk.
Challenges and Future Directions
Despite advances, several challenges remain in the management of Osteogenesis Imperfecta. Long-term effects of pharmacologic agents, optimal dosing regimens, and individualized therapy plans require further study. Genetic therapies are on the horizon, with techniques such as CRISPR/Cas9 offering the potential to correct mutations at the molecular level.
Emerging Therapies
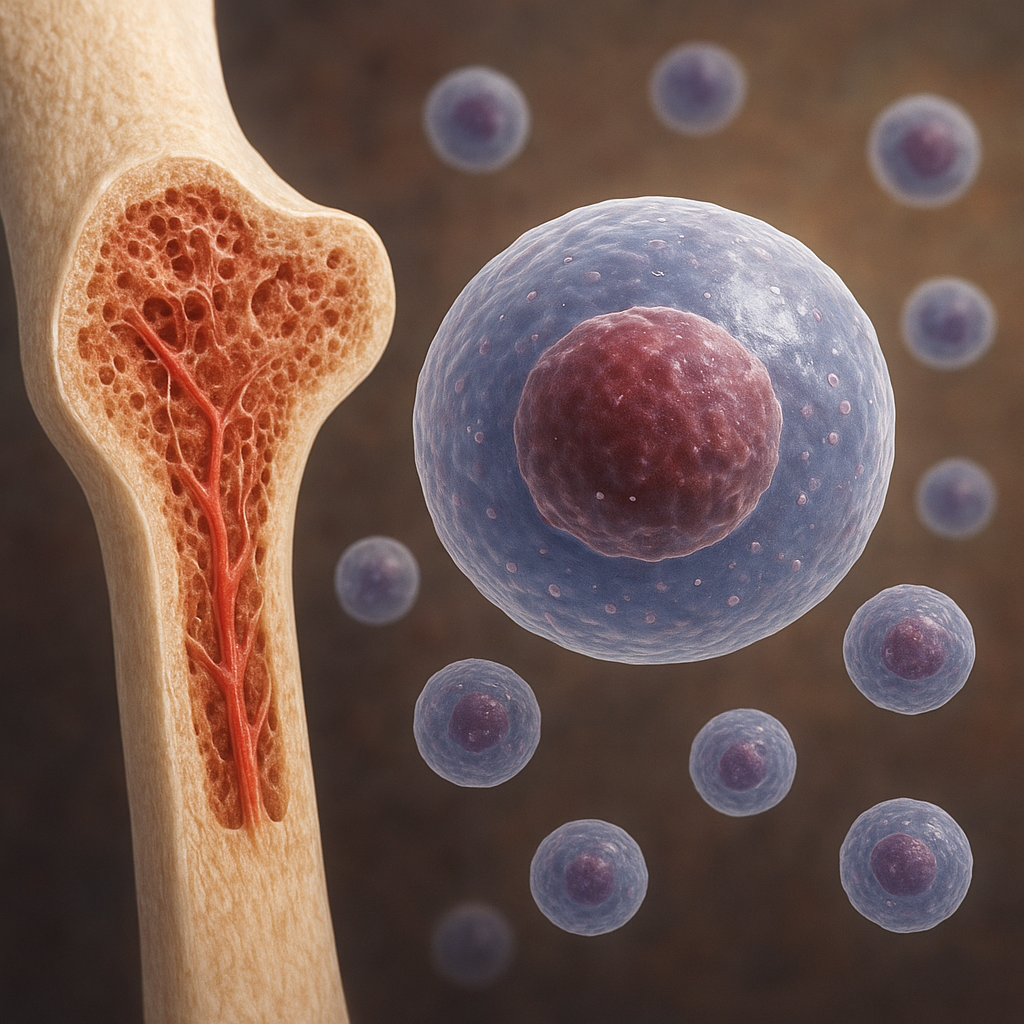
- Gene Editing: Preclinical models demonstrate feasibility of repairing defective collagens genes to restore normal bone architecture.
- Stem Cell Transplantation: Mesenchymal stem cells may contribute to collagen production and bone regeneration.
- Bone Morphogenetic Proteins (BMPs): BMP-2 and BMP-7 are under investigation for their osteoinductive properties and capacity to enhance fracture healing.
Psychosocial Considerations
Living with a chronic skeletal disorder can take a toll on mental health. Access to psychological counseling, peer support networks, and educational resources is crucial. Encouraging patient engagement in decision-making fosters resilience and empowerment.
Long-Term Outlook
With multidisciplinary care and ongoing research, individuals with Osteogenesis Imperfecta can achieve improved mobility, reduced fracture incidence, and enhanced overall well-being. Continued collaboration between clinicians, researchers, and patient advocacy groups will pave the way for novel interventions and a deeper understanding of this multifaceted condition.