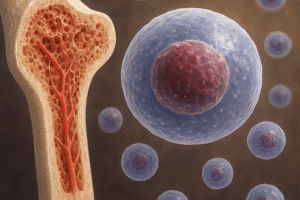
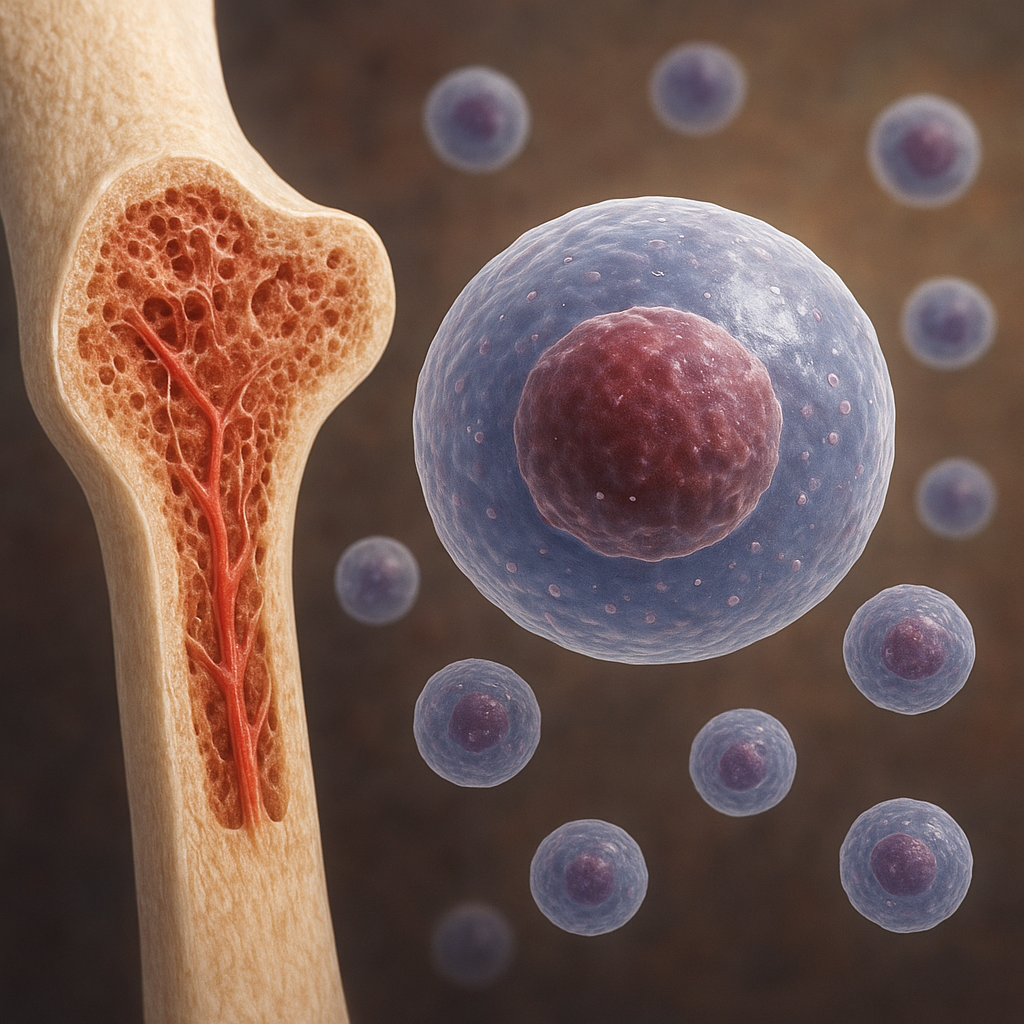
Bone marrow stem cells represent a cornerstone of modern **regenerative** medicine, offering unique capabilities in tissue repair and immune modulation. These multipotent cells, residing in the marrow cavity, have been the subject of extensive research for their potential to restore bone, cartilage, and other tissues. Their versatility derives from two main populations: **hematopoietic** stem cells (HSCs) and mesenchymal stem cells (MSCs). While HSCs give rise to all blood lineages, MSCs possess the remarkable capacity for **differentiation** into osteoblasts, chondrocytes, adipocytes, and more. Understanding the biology, clinical applications, and obstacles of bone marrow-derived stem cells is essential for advancing therapies that can address degenerative bone diseases, traumatic injuries, and immunological disorders.
Biological Characteristics of Bone Marrow Stem Cells
Bone marrow houses two primary stem cell types with distinct roles and characteristics:
- Hematopoietic Stem Cells (HSCs): Responsible for lifelong replenishment of blood and immune cells.
- Mesenchymal Stem Cells (MSCs): Offer multi-lineage **differentiation** potential, particularly toward bone and cartilage.
Hematopoietic Stem Cells
HSCs are defined by their ability to self-renew and generate all blood cell lineages. They express surface markers such as CD34 and CD45, enabling their isolation and enrichment. Following transplantation, HSCs migrate to the bone marrow niche, where they undergo **engraftment** and reconstitute the hematopoietic system. Clinically, HSC transplantation is a well-established therapy for leukemia, lymphoma, and other hematological disorders. The main challenge lies in donor compatibility, graft-versus-host disease (GVHD), and ensuring sufficient cell numbers for successful transplantation.
Mesenchymal Stem Cells
MSCs were initially identified for their ability to form colonies of fibroblast-like cells. They express markers such as CD73, CD90, and CD105, and lack expression of hematopoietic markers. MSCs contribute to tissue repair through:
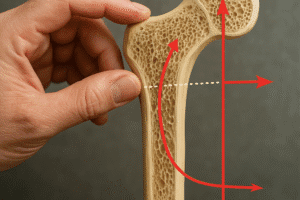
- Osteogenic differentiation: Giving rise to **osteoblasts** for bone regeneration.
- Chondrogenic differentiation: Forming **chondrocytes** for cartilage repair.
- Adipogenic differentiation: Generating **adipocytes**, which can play roles in metabolic regulation.
- Paracrine signaling: Secreting growth factors and cytokines to modulate inflammation and promote **angiogenesis**.
The immunomodulatory properties of MSCs are particularly valuable, as they can suppress T-cell proliferation, regulate dendritic cell maturation, and promote regulatory T-cell expansion. This has led to trials in autoimmune diseases, GVHD prevention, and inflammatory disorders.
Clinical Applications in Orthopedics and Beyond
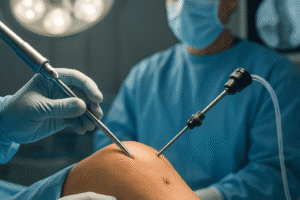
Bone marrow stem cells have moved from the bench to the bedside in various clinical contexts. Research has focused on both autologous and allogeneic **transplantation**, each with advantages and limitations.
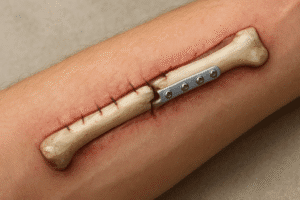
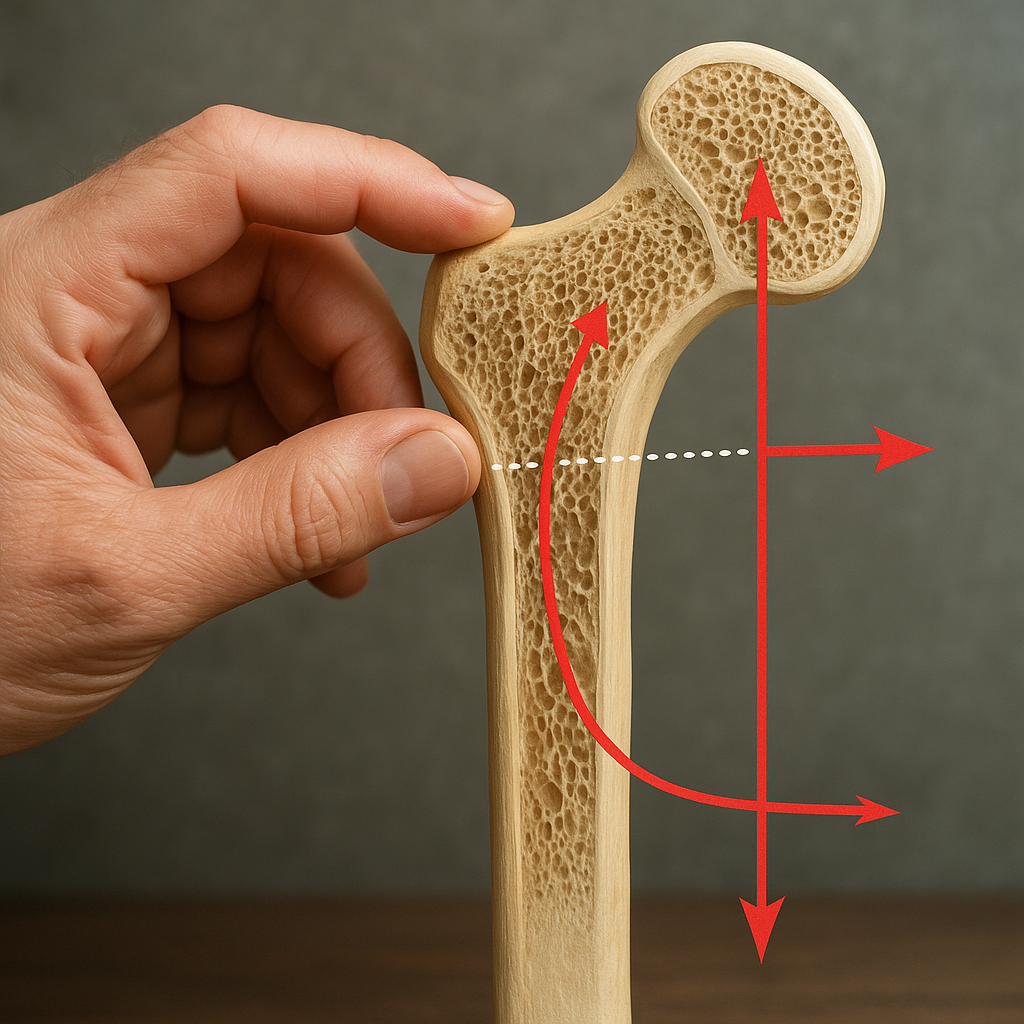
Bone and Cartilage Repair
Orthopedic applications leverage the natural **osteogenesis** and chondrogenic potential of MSCs. Techniques include:
- Direct injection of bone marrow aspirate into fracture non-unions.
- Seeding MSCs onto biodegradable **scaffolds** (e.g., hydroxyapatite or collagen matrices) to reconstruct critical-size bone defects.
- Combining MSCs with growth factors such as bone morphogenetic proteins (BMPs) to enhance bone healing.
Clinical trials have demonstrated improved bone density, reduced healing times, and successful reconstruction of craniofacial defects. Cartilage repair in osteoarthritis patients has shown promising results, with reduced pain and improved joint function following intra-articular MSC injections.
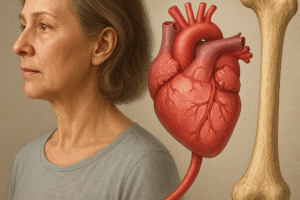
Cardiovascular and Neurological Regeneration
Beyond orthopedics, bone marrow-derived cells have been investigated for:
- Myocardial repair: HSCs and MSCs delivered via intracoronary infusion or direct myocardial injection have shown modest improvements in heart function post-infarction. The mechanisms include neovascularization, paracrine factor release, and potential differentiation into endothelial cells.
- Stroke recovery: MSCs administered intravenously can cross the blood-brain barrier, reduce inflammation, and support neuronal survival, leading to functional recovery in animal models and early human studies.
Immunotherapy and Autoimmune Disorders
HSC transplantation remains the gold standard for certain hematological malignancies. Meanwhile, MSCs are under investigation for:
- Graft-versus-host disease: MSCs can attenuate severe GVHD in transplant recipients.
- Rheumatoid arthritis and systemic lupus erythematosus: Early-phase trials suggest reduced disease activity and lower inflammatory markers following MSC infusion.
- Type I diabetes: Preclinical studies indicate that MSCs may protect pancreatic islet cells and reduce autoimmunity.
Technological Innovations and Future Perspectives
The evolving landscape of bone marrow stem cell therapies is driven by innovative **biomaterials**, genetic engineering, and advanced manufacturing techniques.
3D Bioprinting and Scaffold Engineering
Three-dimensional bioprinting allows the fabrication of complex tissue constructs with precise spatial distribution of cells and materials. Combining MSCs with bioinks composed of natural polymers (e.g., gelatin, fibrin) and inorganic components (e.g., calcium phosphate) yields constructs that mimic native bone architecture. These advances enhance cell viability, **biocompatibility**, and mechanical strength, paving the way for patient-specific grafts.
Gene-Modified Stem Cells
Genetic engineering of MSCs can augment their therapeutic potency. Strategies include:
- Overexpressing angiogenic factors such as VEGF to promote vascularization in ischemic tissues.
- Incorporating anti-inflammatory cytokines like IL-10 to improve immunomodulation.
- Introducing homing receptors (e.g., CXCR4) to enhance targeted migration to injury sites.
These modifications have demonstrated superior functional outcomes in preclinical models, though safety and long-term effects remain under investigation.
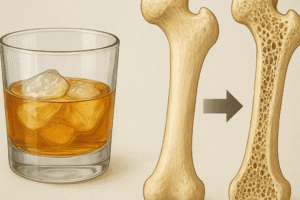
Challenges and Regulatory Considerations
Despite significant progress, several obstacles hinder widespread clinical adoption:
- Cell Source and Yield: Obtaining sufficient MSCs from bone marrow aspirates can be invasive and yield limited cell numbers. Alternative sources (e.g., adipose tissue, umbilical cord) are being explored but differ in potency.
- Standardization: Variability in isolation protocols, culture conditions, and potency assays complicates comparison across studies and regulatory approval.
- Safety Concerns: Risks include ectopic tissue formation, unpredictable differentiation, and potential tumorigenicity, especially with prolonged in vitro expansion or genetic manipulation.
- Regulatory Hurdles: Compliance with Good Manufacturing Practice (GMP), stringent sterility requirements, and comprehensive clinical trial designs add complexity and cost.
Addressing these challenges requires interdisciplinary collaboration among cell biologists, bioengineers, clinicians, and regulatory agencies. Standardized potency assays, robust preclinical models, and carefully designed clinical trials will be essential for translating the promise of bone marrow stem cells into safe and effective therapies.
Key Terms:
- Mesenchymal Stem Cells
- Hematopoietic Stem Cells
- Osteogenesis
- Angiogenesis
- Scaffolds
- Engraftment
- Transplantation
- Immunomodulation
- Differentiation
- Biocompatibility