Minimally invasive orthopedic surgery has sparked a transformative era in musculoskeletal care by reducing soft tissue disruption, accelerating recovery timelines, and enhancing long-term joint function. Surgeons and researchers continue to push the boundaries of technique and technology, integrating novel tools and refined protocols to ensure optimal outcomes. This article explores several key advancements spanning surgical platforms, patient-centered results, postoperative rehabilitation, and the promising horizon of future innovations.
Innovations in Surgical Technology
The quest to minimize collateral damage while maximizing corrective precision has driven the integration of state-of-the-art platforms into routine practice. From robotics and computer-assisted systems to high-definition scopes and navigation software, modern operating rooms now resemble engineering labs as much as clinical suites.
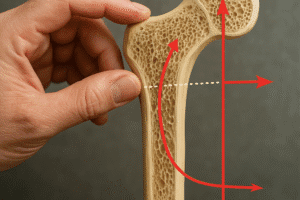
Robotic-Assisted Interventions
Robotic arms and end-effectors deliver controlled, tremor-filtered movements that empower surgeons to perform delicate bone resections and implant placements with sub-millimeter accuracy. These systems often pair with proprietary planning software that enables preoperative templating based on CT or MRI datasets. Key benefits include:
- Enhanced precision in bone cuts and screw trajectories
- Real-time feedback on alignment and ligament tension
- Reduced radiation exposure by integrating preloaded imaging data
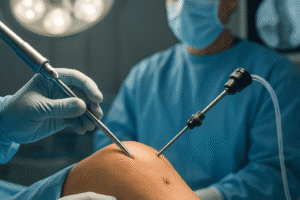
Enhanced Visualization Techniques
Arthroscopic towers equipped with ultra-high-definition cameras and fluid management systems have revolutionized joint inspection. Surgeons gain panoramic views of intra-articular structures via miniature lenses, drastically reducing incision size and soft tissue trauma. Further augmentations include:
- Arthroscopy with 4K or 3D imaging for enhanced depth perception
- Augmented reality overlays that project anatomical landmarks directly onto the surgical field
- Fluoroscopy synchronized with navigation to track instruments in real time
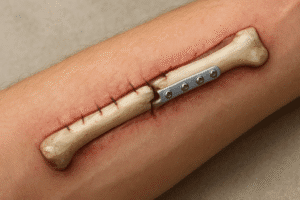
Elevating Patient Outcomes
Delivering superior functional results while ensuring patient comfort remains the central mission of minimally invasive protocols. The combination of technical breakthroughs and optimized perioperative pathways has yielded measurable gains across multiple domains:
- Pain Management: Multimodal analgesia protocols paired with targeted local anesthetic infiltration minimize opioid reliance.
- Reduced Blood Loss: Smaller incisions and meticulous hemostasis lower transfusion rates and related complications.
- Shorter Hospital Stay: Accelerated discharge criteria often allow same-day or next-day ambulation.
- Faster Return to Function: Early weight-bearing and motion exercises promote muscle retention and joint mobility.
Moreover, patient-reported outcome measures consistently highlight elevated patient satisfaction, reflecting the efficacy of less invasive approaches in preserving cosmetic integrity and expediting normal life activities.
Rehabilitation and Biologics Integration
Accelerated Rehabilitation Protocols
Postoperative plans have shifted toward immediate mobilization, leveraging tailored physical therapy regimens that commence within hours of surgery. Principles include:
- Progressive range-of-motion milestones to prevent stiffness
- Resistance training to rebuild periarticular muscle strength
- Neuromuscular re-education exercises to restore proprioception
Digital health platforms and wearable sensors now track patient activity levels, providing clinicians with objective data to refine individual rehabilitation trajectories.
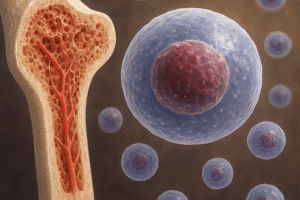
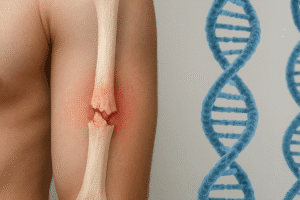
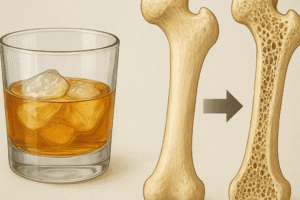
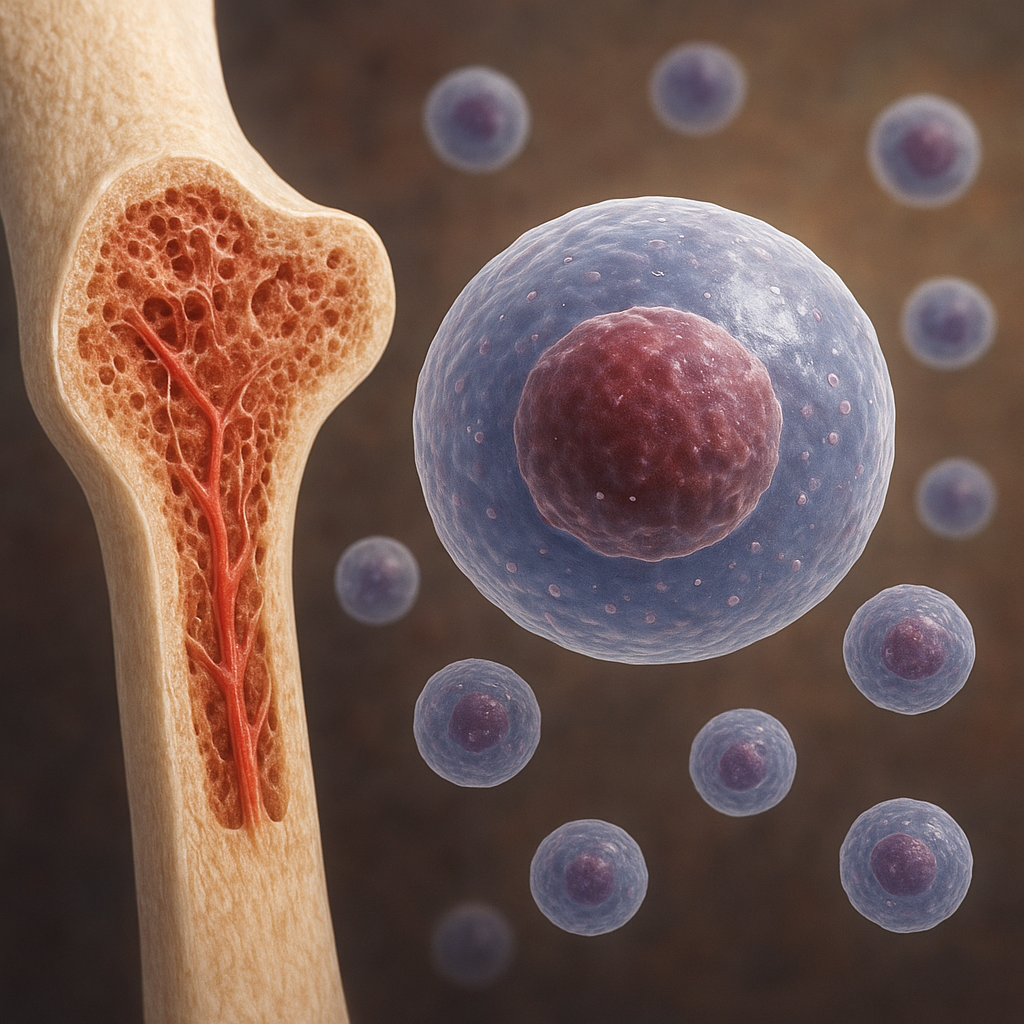
Orthobiologic Enhancements
Introducing biologics during minimally invasive procedures offers a synergistic boost to endogenous healing processes. Strategies encompass:
- Platelet-rich plasma (PRP) injections to release growth factors at the repair site
- Stem cell concentrates seeded onto scaffolds to promote bone and cartilage regeneration
- Matrix-derived biomaterials that provide structural support and guide tissue ingrowth
These adjuncts often complement reduced-invasiveness by accelerating tissue remodeling and potentially lowering the risk of long-term degenerative changes.
Future Outlook and Emerging Trends
As computational power, miniaturization, and materials science continue to evolve, the next decade promises even more ambitious strides. Key areas of anticipated growth include:
- Artificial Intelligence: Machine learning algorithms will refine preoperative planning by predicting optimal implant sizes and assessing patient-specific risk factors.
- Nanotechnology-powered coatings on implants to improve osseointegration and reduce infection rates
- Advanced instrumentation built from lightweight composites that enhance surgeon ergonomics and control
- Telemedicine platforms enabling remote post-surgical monitoring and virtual rehabilitation
Furthermore, integration of multi-omics data—combining genomics, proteomics, and metabolomics—may enable personalized treatment algorithms that optimize both surgical technique and biologic augmentation. Ultimately, ongoing collaboration between engineers, data scientists, and clinicians will define the next frontier, ensuring that minimally invasive orthopedic surgery remains at the cutting edge of patient care.