Bone Morphogenetic Proteins (BMPs) have emerged as pivotal growth factors in the realm of orthopedics and tissue engineering. These multifunctional cytokines play a critical role in the complex process of bone formation and repair, orchestrating cellular events from mesenchymal cell recruitment to differentiation and matrix mineralization. In recent decades, research has focused on harnessing the potent osteoinductive capability of BMPs for clinical use, leading to novel therapies in spine fusion, trauma management, and beyond. This article explores the molecular underpinnings of BMP function, evaluates current medical applications, and outlines emerging strategies that promise safer and more effective bone regeneration approaches.
Biological Mechanisms of Bone Morphogenetic Proteins
Original members of the BMP family were discovered for their ability to induce ectopic osteogenesis when implanted in non-skeletal locations. Today, over 20 BMP isoforms have been identified, each belonging to the transforming growth factor-beta (TGF-β) superfamily. The orchestrated signaling cascade begins when a BMP ligand dimer binds to a heterotetrameric complex of type I and type II serine/threonine kinase receptors on the target cell surface.
SMAD-Dependent Signaling Pathway
- Ligand binding induces type II receptor transphosphorylation of type I receptors.
- Activated type I receptors phosphorylate receptor-regulated SMADs (SMAD1, SMAD5, SMAD8).
- Phosphorylated SMADs form complexes with SMAD4 and translocate to the nucleus.
- Target gene activation drives cell proliferation, differentiation, and extracellular matrix production.
SMAD signaling is tightly regulated by inhibitory SMADs (SMAD6, SMAD7) and extracellular antagonists such as noggin, chordin, and gremlin. This balance ensures proper spatiotemporal control of osteoblast differentiation from mesenchymal stem cells (MSCs), as well as precise bone morphogenesis during embryonic development.
Non-SMAD Pathways and Crosstalk
Beyond SMADs, BMPs engage alternative signaling cascades, including MAPK (p38, ERK, JNK), PI3K/AKT, and Wnt pathways. These non-canonical routes modulate cytoskeletal dynamics, cell migration, and survival, adding layers of control to skeletal patterning. The ability of BMPs to integrate multiple intracellular networks underscores their versatility but also highlights potential risks of off-target effects when applied therapeutically.
Clinical Applications in Bone Repair and Reconstruction
The translation of BMP research into clinical practice has revolutionized certain aspects of orthopedic surgery. Recombinant human BMPs (rhBMPs), produced via advanced DNA recombination technologies, have obtained regulatory approval for specific indications.
Spinal Fusion Procedures
- rhBMP-2 is widely employed in lumbar interbody fusion, enhancing fusion rates compared to autograft alone.
- Clinical trials demonstrate reduced donor site morbidity due to elimination of iliac crest bone harvesting.
- Concerns remain regarding ectopic bone formation and inflammatory reactions at high dose applications.
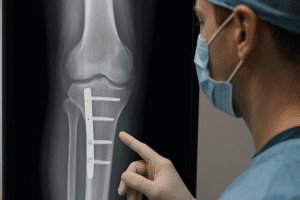
Trauma and Long Bone Nonunions
Chronic nonunions pose a significant challenge in trauma care. Application of rhBMP-7 (osteogenic protein-1) within a carrier matrix promotes vascular infiltration and new bone deposition at fracture sites. Meta-analyses report improved healing rates, particularly in tibial and femoral nonunions, with favorable safety profiles.
Craniofacial and Dental Regeneration
In craniofacial reconstruction, BMPs facilitate alveolar ridge augmentation and repair of congenital deformities. Dental implantology also benefits from localized BMP delivery to enhance osseointegration and keratinized tissue formation around implants.
Advanced Delivery Strategies and Biomaterials
Effective clinical use of BMPs depends on optimized delivery systems that maintain protein bioactivity, control release kinetics, and minimize systemic exposure. A variety of biomaterials and composite carriers have been investigated to satisfy these criteria.
Collagen-Based Matrices
- Porous collagen sponges are the most common BMP carriers, providing a scaffold for cell infiltration.
- Crosslinking methods extend degradation time but may affect growth factor release.
Synthetic Polymers and Hydrogels
Polylactic-co-glycolic acid (PLGA) microspheres encapsulate BMPs, achieving sustained release over weeks. Thermoresponsive hydrogels based on polyethylene glycol (PEG) can be injected in a minimally invasive manner, gelling in situ to provide a customizable 3D network.
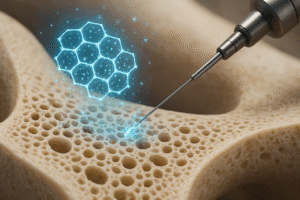
Nanotechnology-Enhanced Systems
- Nanofibrous scaffolds mimic native extracellular matrix architecture, promoting cell adhesion and osteogenic differentiation.
- Functionalization with heparin and other glycosaminoglycans increases BMP binding affinity, reducing required doses.
Challenges and Future Perspectives
Despite significant progress, several challenges impede the broader adoption of BMP-based therapies. High manufacturing costs of recombinant proteins translate into expensive implants, limiting accessibility. Additionally, supraphysiological doses, often necessary to overcome rapid diffusion and inactivation, can lead to complications such as inflammatory edema, heterotopic ossification, and potential oncogenic risks.
Dose Optimization and Safety
Ongoing research aims to refine dosing regimens through improved carriers and localized gene therapy approaches. Viral and non-viral vectors delivering BMP-encoding sequences directly to MSCs could provide sustained, physiological expression, reducing dose spikes and associated adverse events.
Personalized and Regenerative Medicine
In the era of personalized medicine, combining BMPs with patient-derived stem cells and 3D-printed scaffolds may yield custom implants tailored to individual defect geometries. Advances in induced pluripotent stem cell (iPSC) technology further open avenues for autologous cell populations sensitized to BMP cues.
Next-Generation BMP Analogs
Engineering BMP variants with enhanced receptor specificity or lower immunogenicity promises to improve therapeutic indices. Peptide mimetics and small-molecule agonists targeting BMP receptors are under preclinical evaluation, offering potential oral or topical administration routes.
As the field advances, interdisciplinary collaboration among molecular biologists, material scientists, and clinicians will be vital in translating these innovations into safe and effective regenerative treatments, ultimately redefining standards of care in bone and tissue repair.