Rheumatoid arthritis (RA) is a chronic inflammatory disorder that primarily affects the joints, but its impact extends beyond mere discomfort and swelling. This autoimmune condition can lead to significant changes in bone and joint health, resulting in long-term complications. Understanding how rheumatoid arthritis affects bones and joints is crucial for both patients and healthcare providers, as it can guide treatment strategies and improve quality of life.
The Mechanism of Rheumatoid Arthritis
Rheumatoid arthritis is characterized by the immune system mistakenly attacking the synovium, the lining of the membranes that surround the joints. This autoimmune response leads to inflammation, which can cause pain, swelling, and stiffness in the affected areas. Over time, the persistent inflammation can result in damage to the cartilage and bone, leading to joint deformities and loss of function.
Inflammation and Joint Damage
The inflammatory process in RA involves various immune cells, including T cells, B cells, and macrophages, which release pro-inflammatory cytokines. These cytokines, such as tumor necrosis factor (TNF) and interleukin-6 (IL-6), play a significant role in perpetuating inflammation and promoting joint damage. The synovial fluid, which normally lubricates the joints, becomes thickened and inflamed, leading to increased pressure and pain.
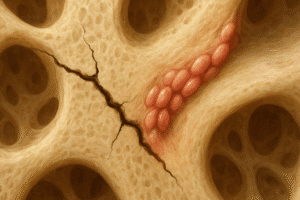
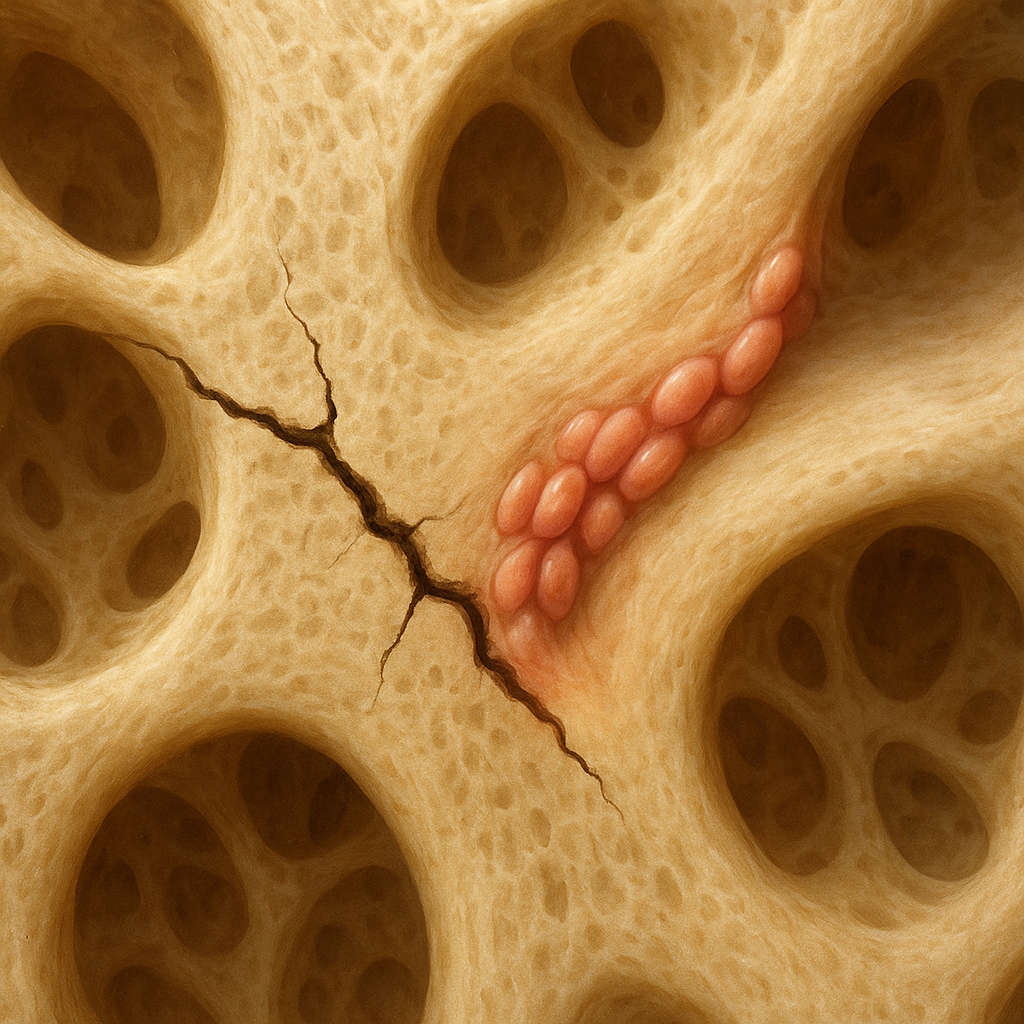
As the disease progresses, the inflammation can erode the cartilage that cushions the joints. Cartilage loss exposes the underlying bone, leading to further complications. The body attempts to repair this damage, but the new bone that forms is often abnormal and can lead to joint deformities. This process is known as bone remodeling, and in RA, it is often dysregulated, resulting in both bone loss and the formation of osteophytes (bone spurs).
Bone Health in Rheumatoid Arthritis
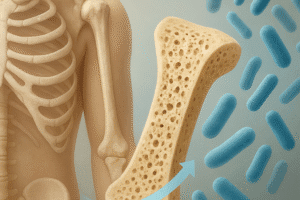
Rheumatoid arthritis not only affects the joints but also has a significant impact on bone health. Patients with RA are at an increased risk of developing osteoporosis, a condition characterized by weakened bones and an increased risk of fractures. The inflammation associated with RA can lead to increased bone resorption, where osteoclasts (cells that break down bone) are more active than osteoblasts (cells that build bone).
Additionally, the use of corticosteroids, a common treatment for RA, can further contribute to bone loss. These medications can inhibit the formation of new bone and increase the risk of fractures. Therefore, it is essential for individuals with RA to monitor their bone health and consider preventive measures, such as calcium and vitamin D supplementation, along with regular weight-bearing exercises.
Managing the Effects of Rheumatoid Arthritis
Effective management of rheumatoid arthritis is crucial to minimize its impact on bones and joints. A comprehensive treatment plan typically includes medication, physical therapy, and lifestyle modifications. Early intervention can help prevent or reduce joint damage and improve overall function.
Medications
Several classes of medications are used to manage rheumatoid arthritis, including nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), and biologics. NSAIDs help reduce pain and inflammation, while DMARDs and biologics target the underlying immune response to slow disease progression.
In addition to these medications, bisphosphonates or other osteoporosis treatments may be prescribed to help protect bone health in patients at risk of fractures. Regular monitoring of bone density can also guide treatment decisions and help prevent complications.
Physical Therapy and Exercise
Physical therapy plays a vital role in managing rheumatoid arthritis. A physical therapist can design a personalized exercise program that focuses on improving joint mobility, strength, and overall function. Low-impact exercises, such as swimming or cycling, can help maintain joint health without putting excessive strain on the affected areas.
Incorporating flexibility and stretching exercises can also help alleviate stiffness and improve range of motion. Patients are encouraged to listen to their bodies and adjust their activity levels as needed to avoid exacerbating their symptoms.
Lifestyle Modifications
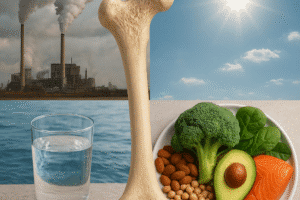
In addition to medical treatment and physical therapy, lifestyle modifications can significantly impact the management of rheumatoid arthritis. Maintaining a healthy weight is essential, as excess weight can place additional stress on the joints. A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and omega-3 fatty acids, can also support overall health and potentially reduce inflammation.
Stress management techniques, such as mindfulness, yoga, or meditation, can help individuals cope with the emotional challenges of living with a chronic condition. Support groups and counseling can provide valuable resources and a sense of community for those affected by rheumatoid arthritis.
Conclusion
Rheumatoid arthritis is a complex condition that significantly affects bones and joints, leading to pain, inflammation, and long-term complications. Understanding the mechanisms behind RA and its impact on bone health is essential for effective management. Through a combination of medication, physical therapy, and lifestyle modifications, individuals with rheumatoid arthritis can take proactive steps to minimize joint damage and maintain their quality of life.
As research continues to advance our understanding of rheumatoid arthritis, new treatment options and strategies will emerge, offering hope for better outcomes for those affected by this challenging condition. Early diagnosis and intervention remain key to preserving joint function and preventing complications, underscoring the importance of awareness and education surrounding rheumatoid arthritis.