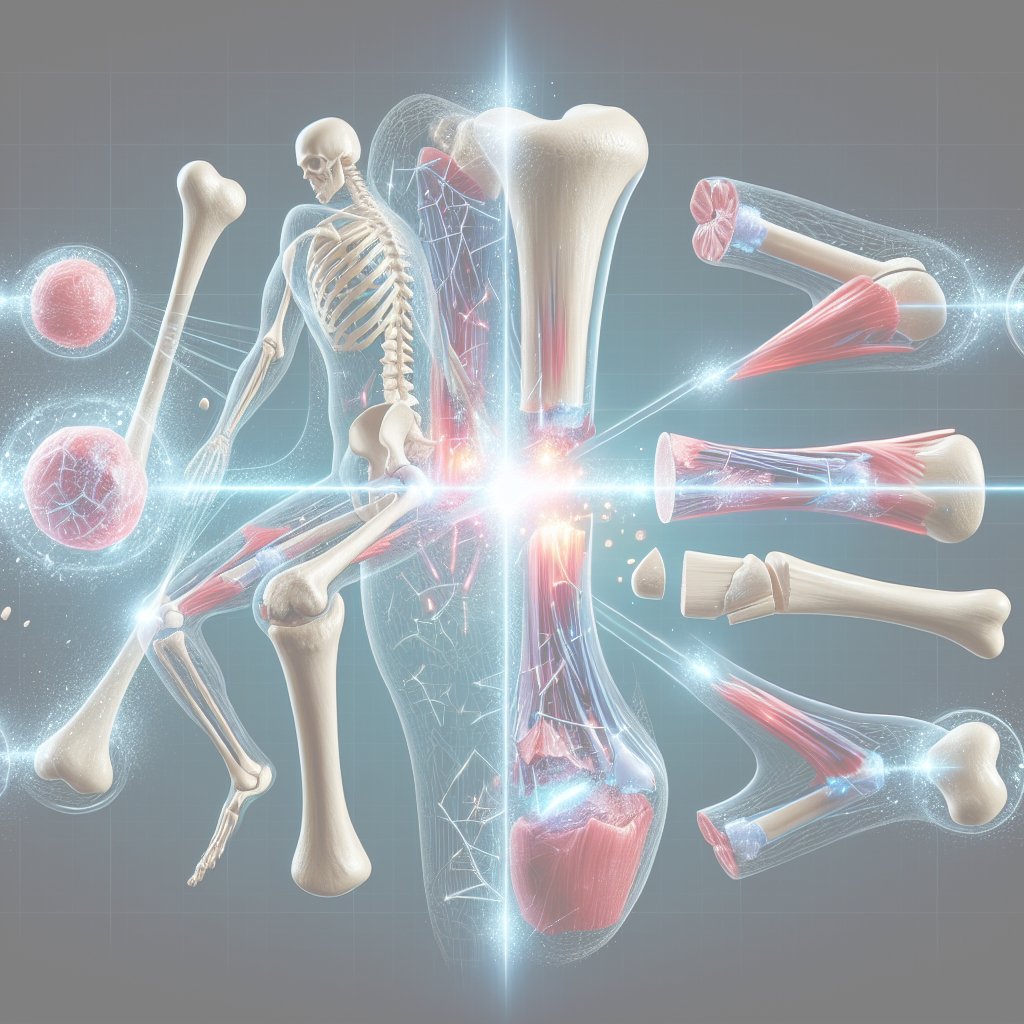
Understanding how fractures heal is a fascinating journey into the intricate processes of bone regeneration. This natural phenomenon not only showcases the remarkable capabilities of the human body but also highlights the importance of proper care and treatment during the healing process. In this article, we will explore the stages of bone healing, the biological mechanisms involved, and the factors that can influence recovery.
The Stages of Bone Healing
Bone healing is a complex process that can be divided into several distinct stages. Each stage plays a crucial role in ensuring that the bone regains its strength and functionality. The three primary stages of bone healing are inflammation, repair, and remodeling.
1. Inflammation
The first stage of bone healing begins immediately after a fracture occurs. This inflammatory response is essential for initiating the healing process. When a bone breaks, the surrounding tissues are damaged, leading to bleeding and the formation of a hematoma (a localized collection of blood). This hematoma serves as a temporary scaffold for the healing process and is rich in growth factors and cytokines that attract various types of cells to the injury site.
During this stage, immune cells, such as macrophages and neutrophils, migrate to the fracture site to clear away debris and prevent infection. These cells release signaling molecules that promote the recruitment of stem cells and other essential cells needed for bone repair. The inflammatory phase typically lasts for several days, setting the stage for the next phase of healing.
2. Repair
The repair phase is characterized by the formation of a soft callus, which eventually transforms into a hard callus. This process begins approximately one week after the fracture occurs. Mesenchymal stem cells differentiate into chondrocytes, which produce cartilage at the fracture site. This cartilage serves as a temporary bridge between the broken ends of the bone.
As the soft callus forms, blood vessels also begin to grow into the area, supplying essential nutrients and oxygen. Over the next few weeks, the cartilage is gradually replaced by woven bone through a process called endochondral ossification. This hard callus provides stability to the fracture and allows for early movement, which is crucial for maintaining joint function.
3. Remodeling
The final stage of bone healing is remodeling, which can take several months to years, depending on the severity of the fracture and the individual’s overall health. During this phase, the hard callus is gradually replaced by lamellar bone, which is stronger and more organized. Osteoclasts, the cells responsible for bone resorption, break down the excess bone formed during the repair phase, while osteoblasts build new bone in a more structured manner.
This remodeling process is influenced by mechanical stress and loading on the bone. As the individual resumes normal activities, the bone adapts to the forces placed upon it, becoming denser and stronger over time. This dynamic process ensures that the bone can withstand future stresses and maintain its integrity.
Factors Influencing Bone Healing
While the stages of bone healing are well understood, several factors can influence the speed and effectiveness of the healing process. These factors can be broadly categorized into biological, mechanical, and environmental influences.
1. Biological Factors
Biological factors play a significant role in bone healing. Age, overall health, and nutritional status can all impact the body’s ability to regenerate bone tissue. For instance, older adults may experience slower healing due to decreased bone density and a reduced capacity for cellular regeneration.
Nutritional deficiencies, particularly in calcium and vitamin D, can also hinder the healing process. Calcium is essential for bone formation, while vitamin D helps regulate calcium absorption. Ensuring adequate intake of these nutrients is crucial for optimal bone healing.
2. Mechanical Factors
The mechanical environment surrounding a fracture significantly influences healing. Proper stabilization of the fracture site is essential to prevent excessive movement, which can disrupt the healing process. Various methods, such as casting, splinting, or surgical fixation, are employed to provide the necessary support during the repair phase.
Additionally, controlled mechanical loading can promote bone healing. Early mobilization and weight-bearing activities, when appropriate, can stimulate bone formation and enhance the remodeling process. However, excessive stress or premature loading can lead to complications, such as nonunion or malunion of the fracture.
3. Environmental Factors
Environmental factors, including smoking, alcohol consumption, and certain medications, can negatively impact bone healing. Smoking has been shown to impair blood flow and reduce the availability of oxygen and nutrients to the healing bone. Similarly, excessive alcohol intake can interfere with the bone remodeling process and increase the risk of complications.
Certain medications, such as corticosteroids, can also affect bone healing by inhibiting the activity of osteoblasts and promoting bone resorption. It is essential for individuals recovering from fractures to discuss their medication use with healthcare providers to ensure optimal healing.
Conclusion
The process of bone healing is a remarkable example of the body’s regenerative capabilities. Understanding the stages of healing and the factors that influence recovery can empower individuals to take an active role in their healing journey. By prioritizing nutrition, adhering to medical advice, and engaging in appropriate physical activity, individuals can support their bodies in the complex process of bone regeneration. As research continues to advance our understanding of bone healing, new treatments and interventions may emerge, further enhancing our ability to promote recovery and improve outcomes for those with fractures.