Assessing bone health requires more than just measuring the mineral content; understanding the complexities of structure, composition, and function can unveil critical insights into skeletal integrity. This article explores innovative approaches to evaluate bone strength beyond conventional density measurements.
The Limitations of Bone Mineral Density
Bone Mineral Density (BMD) has long been the clinical cornerstone for diagnosing osteoporosis and estimating fracture risk. While dual-energy X-ray absorptiometry (DXA) provides a reliable measure of mineral content per area, several important aspects of bone quality remain unaddressed:
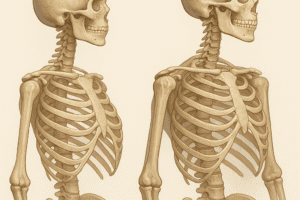
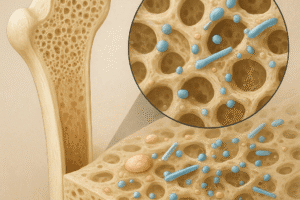
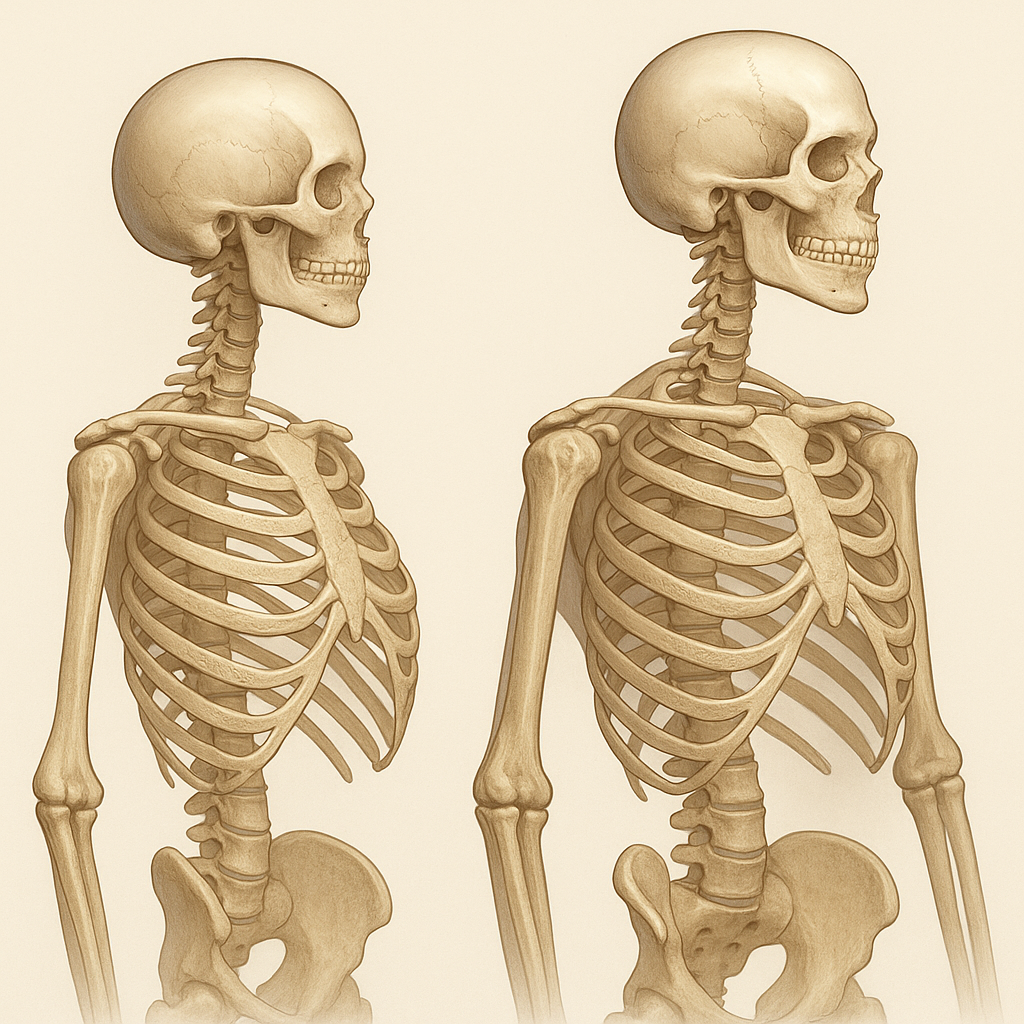
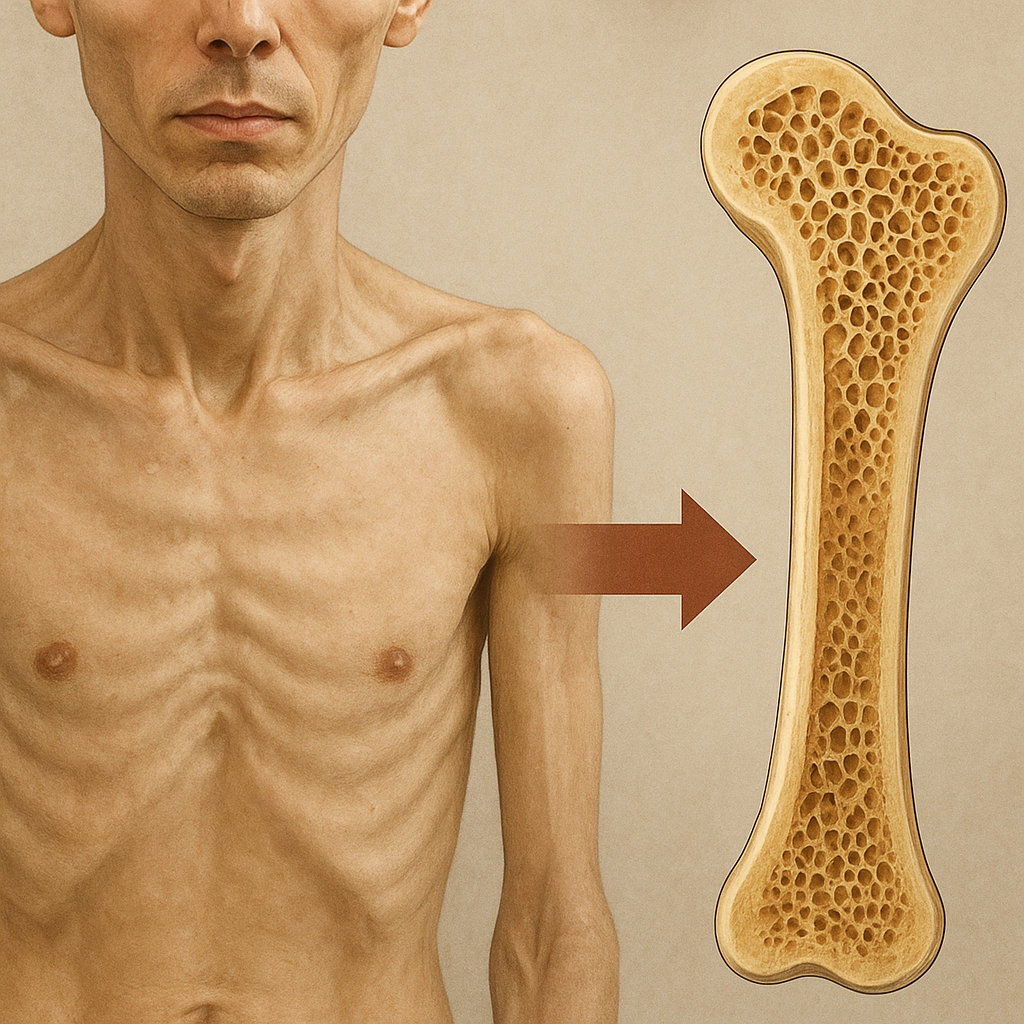
- Microarchitecture: The spatial arrangement of trabeculae and cortical porosity significantly influences mechanical competence, yet BMD cannot discern these fine-scale details.
- Material Properties: Elasticity, toughness, and mineralization heterogeneity play roles in energy absorption during trauma, aspects that density alone overlooks.
- Bone Geometry: Cross-sectional area, cortical thickness, and moment of inertia are critical determinants of load-bearing capacity, independent of mineral content.
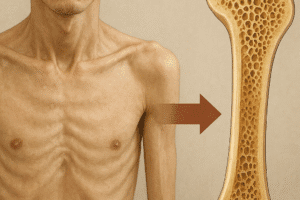
Consequently, relying solely on BMD risks underestimating fracture risk in individuals with atypical bone geometry or compromised material quality. Clinicians and researchers must look beyond density to capture a comprehensive picture of skeletal health.
Advanced Imaging Techniques
Recent technological advances have expanded our toolkit for skeletal evaluation. High-resolution modalities and computational methods reveal hidden features of bone strength:
High-Resolution Peripheral Quantitative Computed Tomography
HR-pQCT enables in vivo visualization of trabecular and cortical microarchitecture at a voxel size of up to 82 micrometers. This level of detail permits analysis of parameters such as trabecular thickness, separation, and number. Studies demonstrate that HR-pQCT-derived metrics correlate more strongly with fracture history than DXA-derived BMD.
Magnetic Resonance Imaging
MRI offers radiation-free assessment of bone and surrounding soft tissue. Sequences optimized for bone water content and collagen matrix density provide insights into bone resilience and quality. Combining morphological and functional MRI techniques can detect early changes in bone composition before significant mineral loss occurs.
Finite Element Analysis
By converting HR-pQCT or MRI datasets into computational models, finite element analysis (finite element analysis) estimates mechanical behavior under simulated loads. These models calculate parameters like stiffness, failure load, and stress distribution, offering a virtual biomechanical assessment that complements imaging findings.
Biochemical Markers and Functional Assessments
Biochemical and functional approaches provide dynamic information on bone turnover and strength adaptation. When paired with structural imaging, they yield a more holistic evaluation:
Bone Turnover Markers
Serum and urine biomarkers reflect the rates of bone formation and resorption. Key markers include:
- Procollagen type I N-terminal propeptide (PINP), indicating osteoblastic activity.
- C-terminal telopeptide of type I collagen (CTX), reflecting osteoclastic resorption.
Monitoring these biomarkers can inform therapeutic efficacy and predict rapid changes in bone strength that may not yet affect BMD or structure.
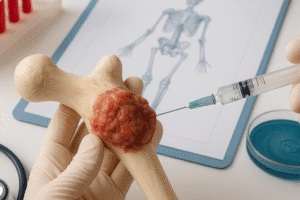
Mechanical Testing of Biopsies
In research settings, small transiliac bone biopsies undergo mechanical testing for yield strength and toughness. Microindentation techniques, such as Reference Point Indentation (RPI), gauge bone tissue hardness and crack propagation resistance. These measures illuminate material characteristics that imaging alone cannot capture.
Functional Performance Tests
Physical performance assessments correlate with bone strength by evaluating muscle-bone interactions and fall risk. Common tests include:
- Timed Up and Go (TUG) test for mobility and balance.
- Grip strength measurement as a surrogate for overall musculoskeletal health.
- Gait speed and stair-climb tests to assess lower limb function.
Combining functional data with structural and biochemical metrics enhances fracture risk prediction beyond BMD.
Clinical Implications and Future Directions
Integrating advanced measures of bone quality into routine practice remains a challenge due to cost, accessibility, and standardization issues. However, the potential benefits include:
- Personalized Treatment: Tailoring therapy based on individual bone geometry, microarchitecture, and turnover rates rather than relying solely on density thresholds.
- Early Intervention: Detecting subtle changes in bone quality before significant mineral loss could enable preventive strategies to avert progression to clinical osteoporosis.
- Improved Risk Stratification: Combining imaging, quantitative biomechanical models, and biomarkers to refine fracture risk algorithms, especially in patients with secondary bone disorders such as diabetes or chronic glucocorticoid use.
Future research will likely focus on miniaturized, point-of-care devices for bone strength evaluation, novel biomechanics sensors embedded in wearable technology, and artificial intelligence models that integrate multi-modal data streams. By embracing a multi-faceted approach to skeletal health, clinicians can provide more accurate diagnoses and effective, individualized therapies that move beyond the confines of bone density.