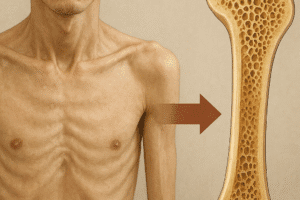
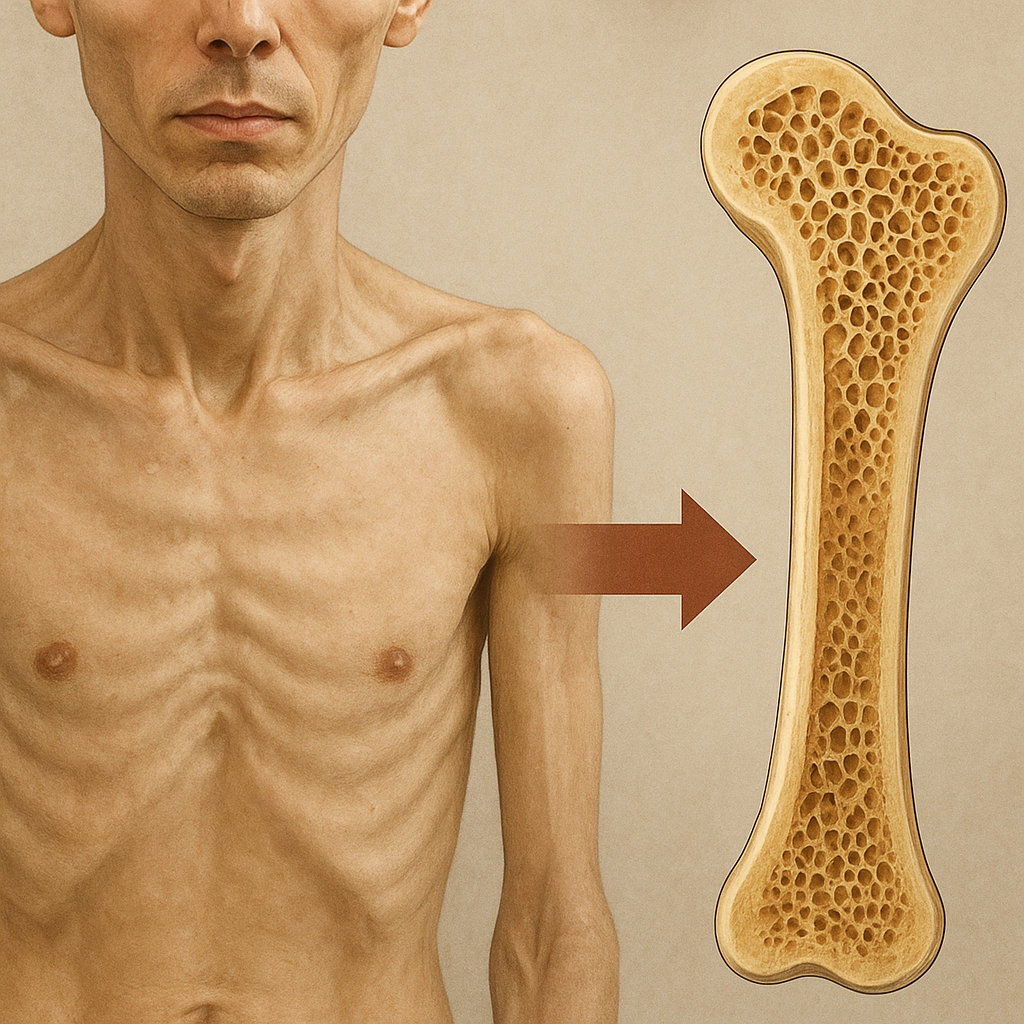
Malnutrition represents a critical yet often overlooked factor in the development of bone disorders. When the body lacks essential nutrients, the intricate process of bone remodeling is disrupted, leading to compromised skeletal integrity. This article explores how insufficient dietary intake of key elements undermines bone strength, elevates fracture risk, and sets the stage for chronic conditions such as osteoporosis. By examining the underlying biological mechanisms, clinical manifestations, and effective nutritional interventions, healthcare professionals can better address the hidden epidemic of bone weakness fueled by poor nutrition.
Nutritional Deficiencies and Their Impact on Bone Formation
Healthy bones depend on a delicate balance of mineralization and cellular turnover. The role of micronutrients and macronutrients in this process cannot be overstated. When dietary supply falls short, the skeletal system becomes vulnerable to defects that may manifest early in life or emerge gradually with aging.
Macronutrient Insufficiency
Protein serves as the primary building block for collagen, the organic matrix that imparts flexibility and toughness to bone tissue. Inadequate protein intake slows down osteoblast activity, reducing collagen synthesis and leaving bones brittle. Similarly, insufficient caloric consumption forces the body to catabolize muscle and compromise bone maintenance, further diminishing bone density.
Key Micronutrients
- Calcium: Fundamental for hydroxyapatite formation. A persistent deficit leads to demineralization and structural weaknesses.
- Vitamin D: Essential for calcium absorption. Deficiency impairs mineral uptake, directly undermining bone mineral content.
- Phosphorus, Magnesium, Zinc: Cofactors in enzymatic reactions crucial for bone matrix formation and mineral deposition.
- Vitamin K: Supports the carboxylation of osteocalcin, a protein involved in binding calcium to the bone matrix.
Mechanisms of Bone Weakening in Malnourished Individuals
Understanding the pathophysiological pathways triggered by malnutrition is essential for targeted therapies. These mechanisms span hormonal disruption, altered metabolism, and direct cellular impairment.
Endocrine Dysregulation
Chronic undernutrition disrupts the endocrine axis, reducing levels of growth hormone and sex steroids. These hormones promote osteoblast proliferation and inhibit osteoclast-mediated bone resorption. Their decline shifts the remodeling balance toward bone loss, accelerating the onset of osteoporosis even in younger populations.
Altered Mineral Metabolism
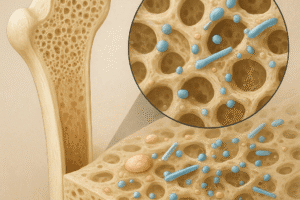
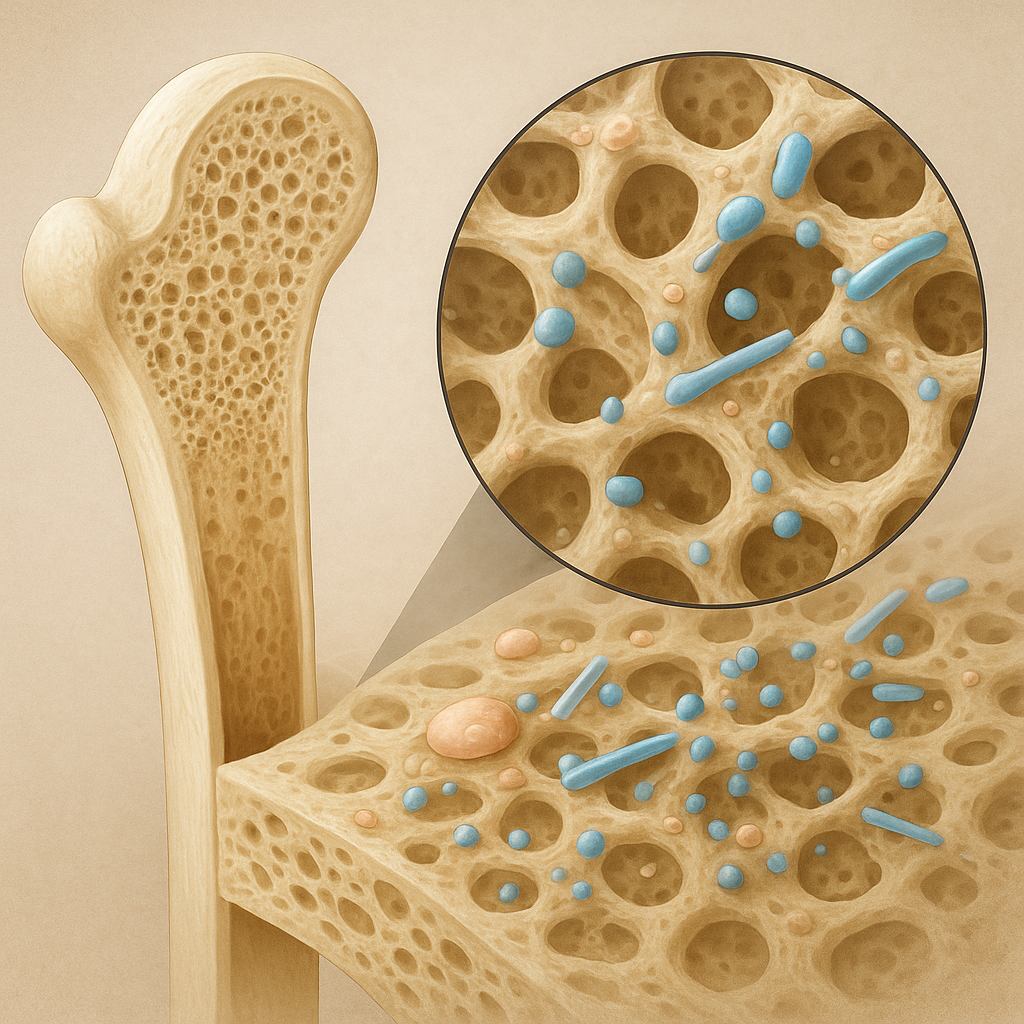
Low calcium intake, compounded by vitamin D deficiency, triggers secondary hyperparathyroidism. Elevated parathyroid hormone (PTH) levels enhance osteoclast activity to mobilize calcium from bone, leading to trabecular thinning and cortical porosity. Over time, this metabolic adjustment becomes maladaptive, resulting in progressively weaker bones.
Cellular and Molecular Effects
At the cellular level, nutrient shortages impair the proliferation and differentiation of osteoprogenitor cells. Mitochondrial dysfunction due to a lack of essential vitamins and minerals further reduces energy supply, hampering the synthesis of collagen and non-collagenous proteins that form the organic scaffold of bone. Inflammatory cytokines, often elevated in undernourished states, exacerbate osteoclastogenesis and bone degradation.
Clinical Implications and Preventive Strategies
The consequences of bone weakening range from subtle microarchitectural changes to overt fragility fractures. Clinicians must recognize the multifactorial roots of skeletal demineralization and implement comprehensive prevention and treatment plans.
Risk Assessment and Early Detection
- BMD Measurements: Dual-energy X-ray absorptiometry (DXA) remains the gold standard for evaluating bone density.
- Biochemical Markers: Serum calcium, 25-hydroxyvitamin D, PTH, and bone turnover markers provide insights into ongoing metabolic alterations.
- Nutritional Screening: Detailed dietary histories and anthropometric assessments identify individuals at risk of chronic undernutrition.
Dietary and Lifestyle Modifications
Promoting a balanced diet rich in calcium and vitamin D is the cornerstone of prevention. Sources include dairy products, leafy greens, fortified cereals, and fatty fish. Incorporating adequate protein from lean meats, legumes, and nuts supports the collagen matrix. Regular weight-bearing exercise further stimulates bone formation and enhances muscle strength, reducing falls and fracture risk.
Supplementation and Pharmacological Support
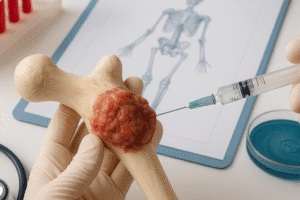
When dietary intake fails to meet needs, targeted supplementation becomes necessary. Calcium carbonate or citrate combined with vitamin D3 ensures proper absorption. In severe cases, anabolic agents such as teriparatide may be prescribed to boost osteoblast activity. Bisphosphonates, though primarily antiresorptive, can stabilize bone mass in individuals with advanced osteoporosis resulting from long-term malnutrition.
Emerging Research and Future Directions
Ongoing studies aim to unravel novel pathways by which malnutrition compromises bone health and to develop innovative interventions. Advances in nutrigenomics explore how individual genetic profiles influence nutrient requirements and bone responses. Additionally, investigations into gut microbiota reveal its role in modulating calcium absorption and systemic inflammation, presenting new opportunities for probiotic therapies.
Bone Regeneration and Tissue Engineering
Biomaterials enriched with growth factors and stem cell therapies show promise in reconstructing bone defects in malnourished individuals. These cutting-edge approaches seek to overcome the impaired healing capacity characteristic of nutrient-deprived states.
Public Health Initiatives
Addressing malnutrition at the population level involves fortification programs, educational campaigns, and improved access to nutrient-rich foods. Collaboration between healthcare providers, government agencies, and community organizations is vital for reducing the global burden of bone weakness linked to dietary insufficiencies.