The intricate interplay between the immune system and skeletal tissues has redefined our understanding of bone repair. Far from serving solely as a structural framework, bone is actively involved in dynamic processes mediated by immune cells, soluble factors, and signaling pathways. Insights into these mechanisms not only enrich basic science but also pave the way for novel therapies in orthopedics and regenerative medicine.
Overview of Bone Repair Mechanisms
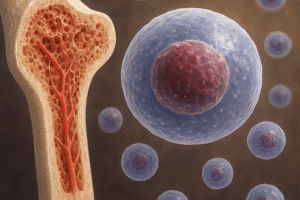
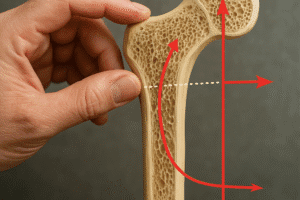
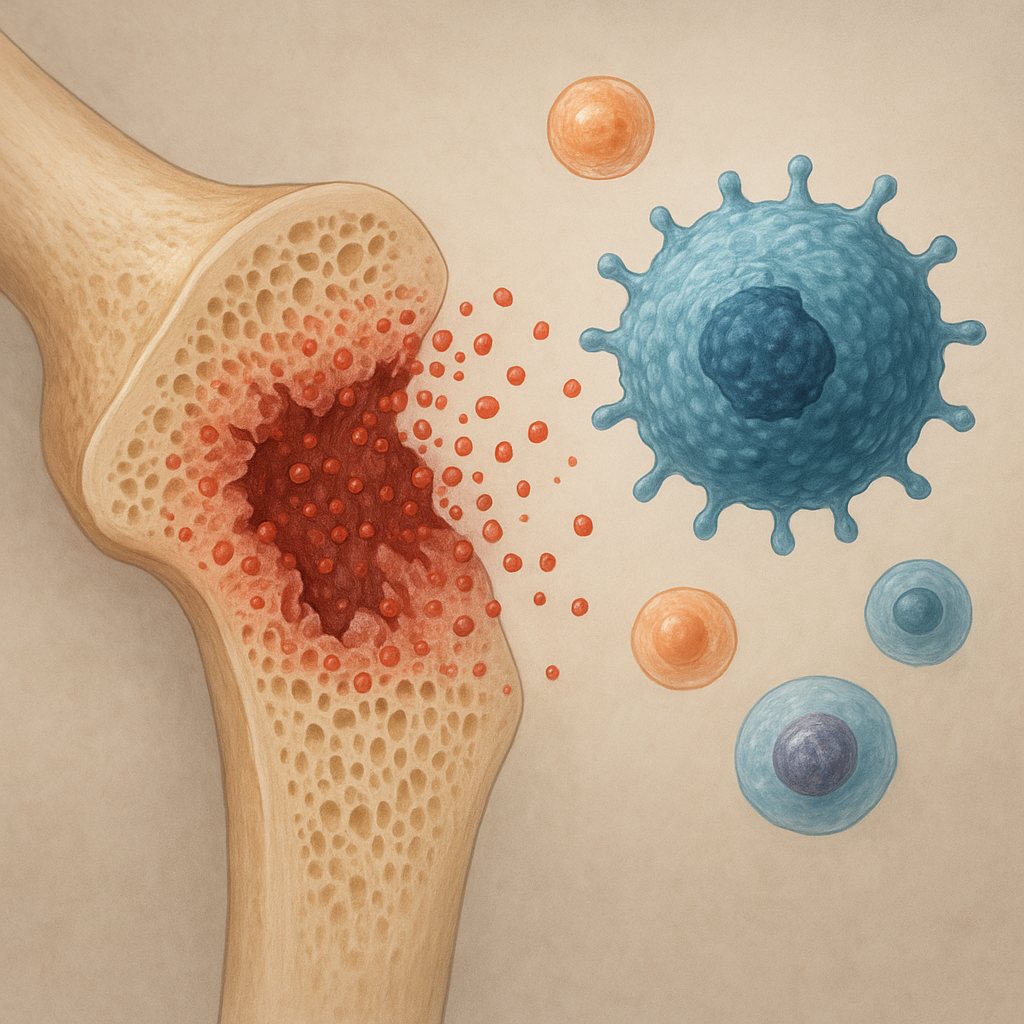
Bone healing is typically described in three overlapping stages: hematoma formation and inflammation, soft callus formation and regeneration, and hard callus remodeling leading to restored mechanical integrity. The first phase, triggered immediately after injury, involves vascular disruption and the recruitment of circulating leukocytes. This influx sets the stage for debris clearance and the release of growth factors that orchestrate subsequent events.
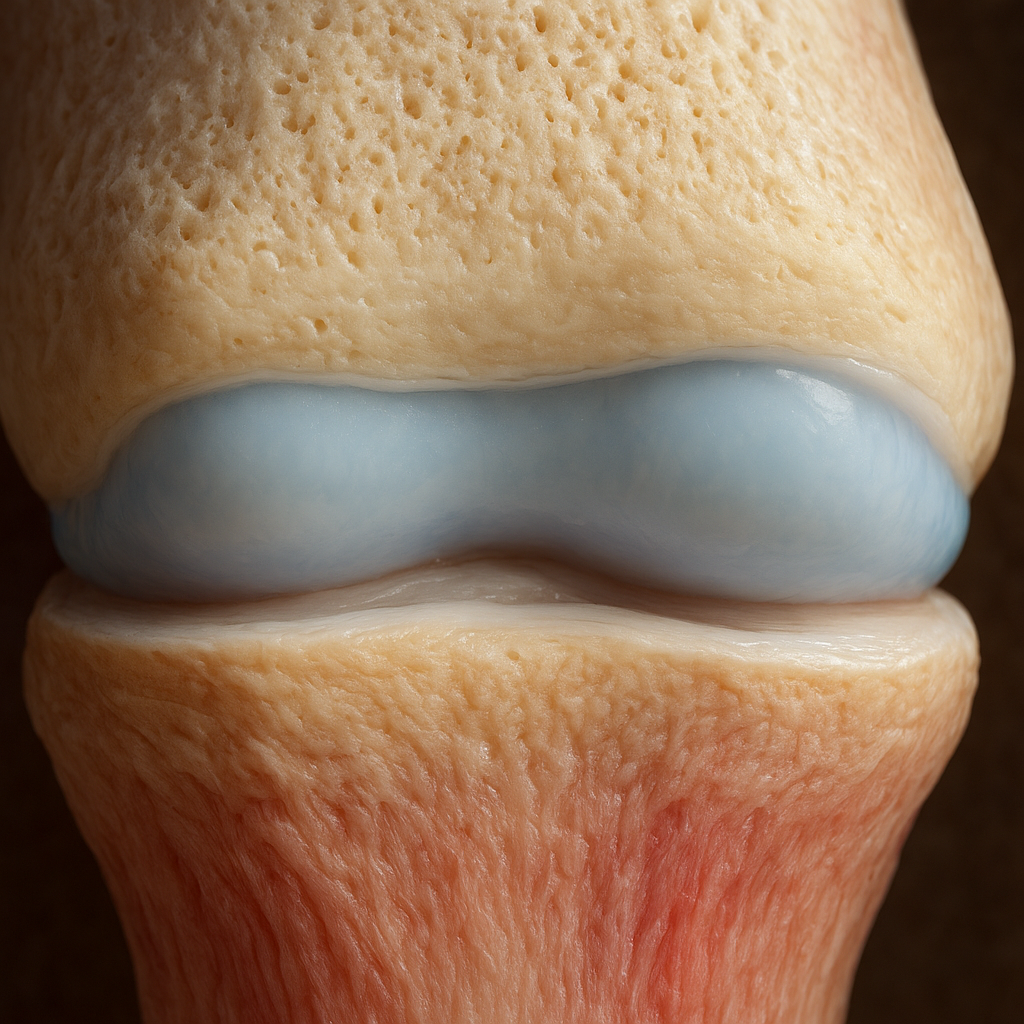
During the reparative stage, mesenchymal stem cells (MSCs) differentiate into osteoblasts that synthesize new bone matrix. Concurrently, chondrogenesis occurs to form a cartilaginous template that is later replaced by endochondral bone. Finally, the remodeling phase is characterized by the balanced actions of osteoclasts resorbing mineralized tissue and osteoblasts rebuilding lamellar bone. This phase restores the original bone microarchitecture and ensures long-term homeostasis.
Immune Cells and Their Functions in Bone Healing
Macrophages and Neutrophils
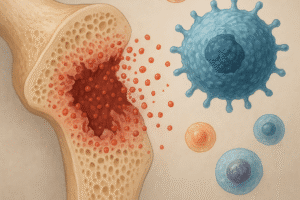
Macrophages are among the first responders at the injury site. They transition from a pro-inflammatory M1 phenotype that clears pathogens and necrotic debris to an anti-inflammatory M2 phenotype that promotes tissue repair. The sequential shift between these states is critical: prolonged M1 activity can lead to chronic inflammation, while premature M2 dominance may compromise microbial defense.
- M1 macrophages release high levels of cytokines such as TNF-α and IL-6, essential for early immune activation.
- M2 macrophages produce IL-10 and TGF-β, which support MSC recruitment and matrix deposition.
Neutrophils, although short-lived, contribute by releasing proteases and reactive oxygen species. Their timely apoptosis and phagocytosis by macrophages are essential steps that transition the environment from inflammatory to regenerative.
T and B Lymphocytes
T lymphocytes modulate osteogenesis through cytokine secretion and direct cell–cell contact. Th17 cells produce IL-17, which can enhance osteoclastogenesis, whereas regulatory T cells (Tregs) secrete IL-10, restraining excessive bone resorption. The balance between effector and regulatory subsets influences healing outcomes.
B lymphocytes are traditionally linked to humoral immunity, but they also secrete osteoprotegerin (OPG), a decoy receptor that binds to receptor activator of nuclear factor κB ligand (RANKL), thus inhibiting osteoclast differentiation. By modulating the RANK/RANKL/OPG axis, B cells can directly affect the remodeling phase.
Other Innate Immune Players
Natural killer cells and dendritic cells also take part in bone repair, albeit their roles are less well-defined. NK cells can lyse senescent or infected cells, while dendritic cells influence T cell polarization through antigen presentation and cytokine profiles.
Molecular Signaling Pathways Bridging Immunity and Osteogenesis
Diverse signaling networks integrate immune cues with bone-forming processes. Among the most prominent are the RANK/RANKL/OPG triad, bone morphogenetic proteins (BMPs), and the Wnt/β-catenin pathway.
RANK/RANKL/OPG Axis
The interaction between RANKL on osteoblast-lineage cells and RANK on osteoclast precursors is essential for osteoclastogenesis. OPG, produced by osteoblasts and B cells, competitively inhibits this binding. Immune-derived cytokines modulate the expression of these molecules: for instance, IL-1 and IL-17 upregulate RANKL, thereby favoring bone resorption, whereas IL-10 induces OPG synthesis, protecting bone mass.
BMP and Wnt Signaling
BMPs are growth factors that trigger MSC differentiation toward osteogenic and chondrogenic lineages. Several BMP family members are upregulated in response to inflammatory stimuli. The Wnt pathway, essential for osteoblast maturation and function, is influenced by immune cells through the secretion of Wnt antagonists such as DKK1 and sclerostin. Aberrant Wnt inhibition by inflammatory mediators can impair bone formation and compromise healing.
Crosstalk via Chemokines and Adhesion Molecules
Chemokines such as CXCL12 govern the homing of MSCs and leukocytes to injury sites. Adhesion molecules (e.g., integrins and selectins) facilitate cell–matrix and cell–cell interactions, ensuring that immune cells and osteoprogenitors coordinate effectively. Disruption of these interactions can delay or derail the repair process.
Clinical Implications and Therapeutic Perspectives
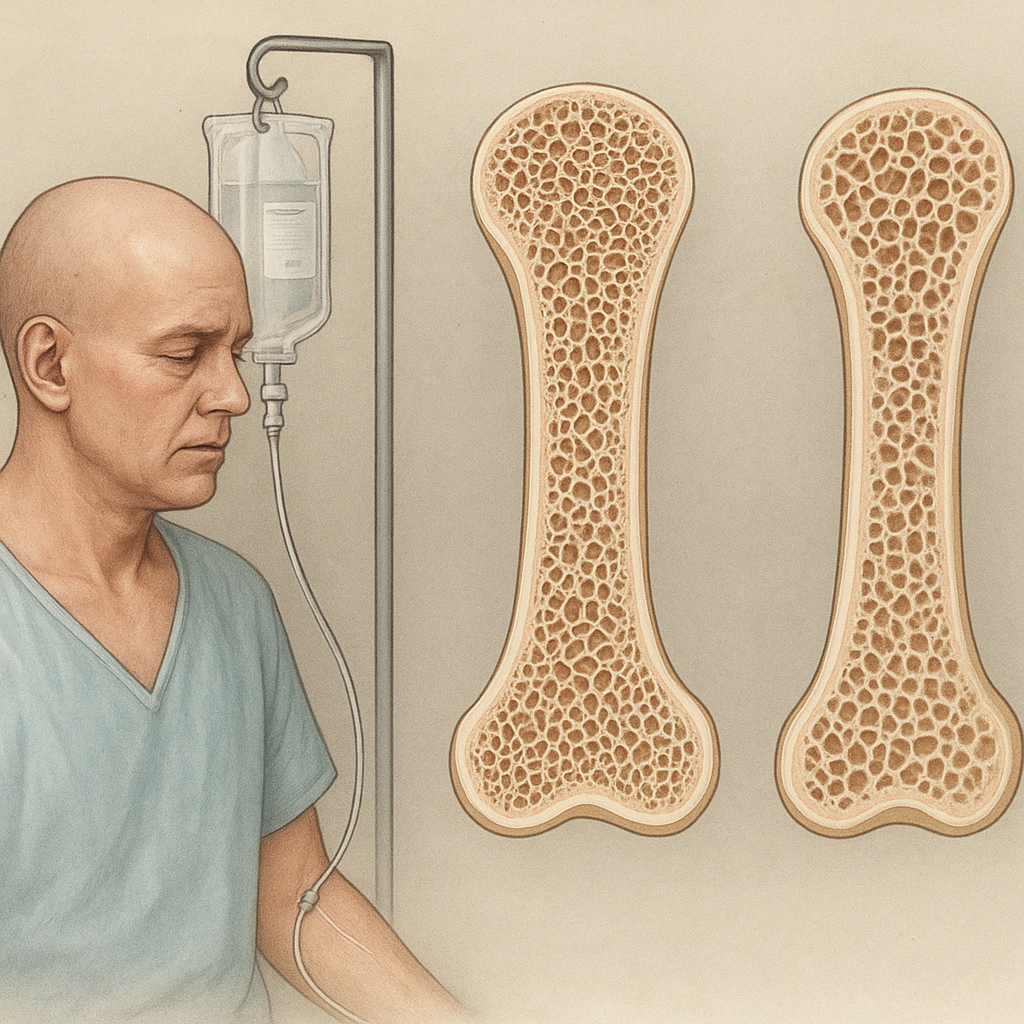
Understanding immune–bone interactions has immediate translational relevance. Inflammatory bone diseases, such as rheumatoid arthritis and periodontitis, involve dysregulated immune responses that lead to excessive bone loss. Targeting cytokines (e.g., anti-TNF agents) or signaling pathways (e.g., RANKL inhibitors) has already improved patient outcomes.
Emerging strategies aim to harness immunomodulation for enhanced fracture repair. Biomaterials loaded with immunoregulatory agents—such as IL-4 to promote M2 macrophage polarization—or scaffolds that release osteoinductive BMPs in a controlled manner can accelerate healing. Moreover, cell-based therapies employing MSCs preconditioned with immune-derived stimuli show promise in preclinical models.
Advancements in bioengineering, including 3D-printed implants with tailored surface chemistries, further illustrate how manipulating the local immune milieu can direct regenerative processes. Personalized medicine approaches, taking into account patient-specific immune profiles, will optimize treatment strategies and minimize complications.