The connection between bone health and chronic illnesses such as diabetes is a complex and multifaceted issue that has garnered increasing attention in recent years. As the prevalence of chronic diseases rises globally, understanding how these conditions impact bone density and overall skeletal health becomes crucial. This article delves into the intricate relationship between bone health and diabetes, exploring the underlying mechanisms, the implications for patient care, and strategies for maintaining optimal bone health in individuals with chronic illnesses.
Understanding Bone Health
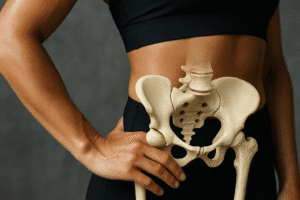
Bone health is a critical aspect of overall well-being, as bones provide structure, protect organs, and facilitate movement. The skeletal system undergoes a continuous process of remodeling, where old bone tissue is replaced by new bone tissue. This process is influenced by various factors, including nutrition, physical activity, hormonal balance, and the presence of chronic diseases.
Bone density, a measure of the amount of mineral matter per square centimeter of bone, is a key indicator of bone health. Low bone density can lead to conditions such as osteoporosis, increasing the risk of fractures and other complications. Maintaining healthy bones requires a balanced diet rich in calcium and vitamin D, regular weight-bearing exercise, and avoiding harmful habits such as smoking and excessive alcohol consumption.
The Impact of Diabetes on Bone Health
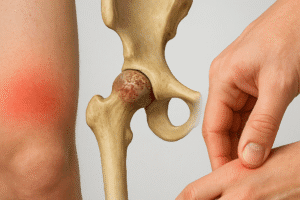
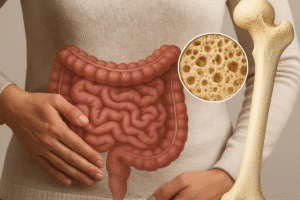
Diabetes, particularly type 2 diabetes, has been linked to various complications that can adversely affect bone health. Research indicates that individuals with diabetes may experience changes in bone density and quality, leading to an increased risk of fractures. Several mechanisms contribute to this relationship:
- Metabolic Changes: Diabetes alters the metabolism of calcium and phosphorus, essential minerals for bone health. Insulin resistance, a hallmark of type 2 diabetes, can disrupt the balance of these minerals, negatively impacting bone remodeling.
- Inflammation: Chronic inflammation associated with diabetes can impair the function of osteoblasts (bone-forming cells) and osteoclasts (bone-resorbing cells), leading to an imbalance in bone remodeling and reduced bone density.
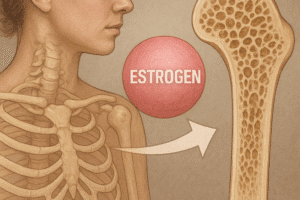
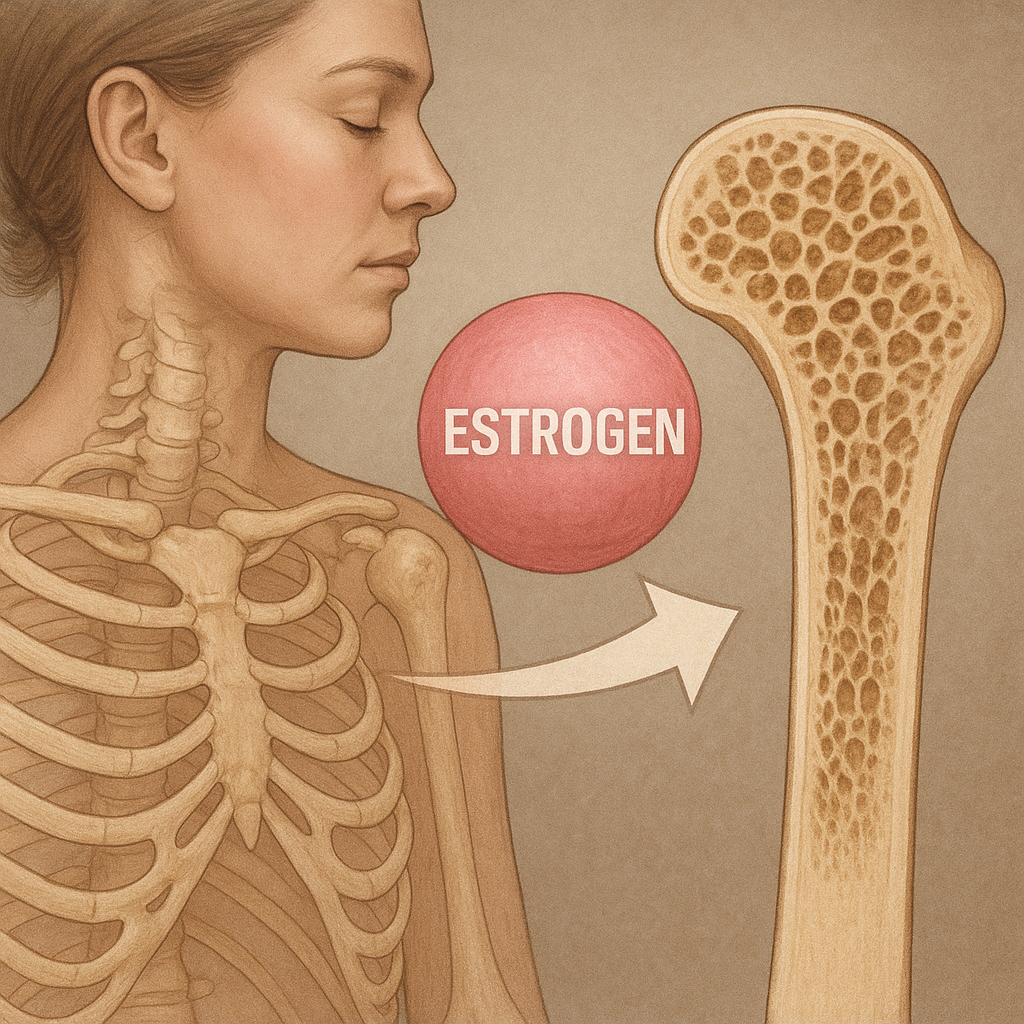
- Hormonal Factors: Diabetes can affect the levels of hormones that regulate bone metabolism, such as insulin, glucagon, and sex hormones. These hormonal changes can contribute to decreased bone strength and increased fracture risk.
- Neuropathy: Diabetic neuropathy, a common complication of diabetes, can lead to balance issues and an increased risk of falls, further heightening the risk of fractures.
Clinical Implications
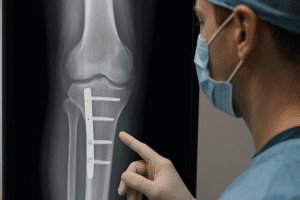
Understanding the link between diabetes and bone health is essential for healthcare providers in managing patients with chronic illnesses. Regular screening for bone density in individuals with diabetes can help identify those at risk for osteoporosis and fractures. Early intervention strategies, including lifestyle modifications and pharmacological treatments, can significantly improve bone health outcomes.
Healthcare providers should emphasize the importance of a balanced diet rich in calcium and vitamin D, as well as the role of regular physical activity in maintaining bone health. Weight-bearing exercises, such as walking, jogging, and resistance training, can help strengthen bones and improve overall physical function.
Strategies for Maintaining Bone Health in Diabetic Patients
For individuals with diabetes, maintaining bone health requires a proactive approach. Here are several strategies that can be implemented:
- Nutrition: A diet rich in calcium and vitamin D is crucial. Foods such as dairy products, leafy greens, and fortified foods should be included. Additionally, adequate protein intake is essential for bone health.
- Physical Activity: Engaging in regular weight-bearing and resistance exercises can help improve bone density and strength. Activities such as walking, dancing, and strength training are beneficial.
- Fall Prevention: Implementing fall prevention strategies, such as home modifications and balance training, can reduce the risk of fractures in individuals with diabetes.
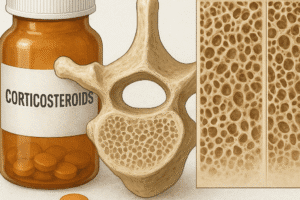
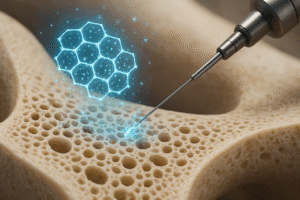
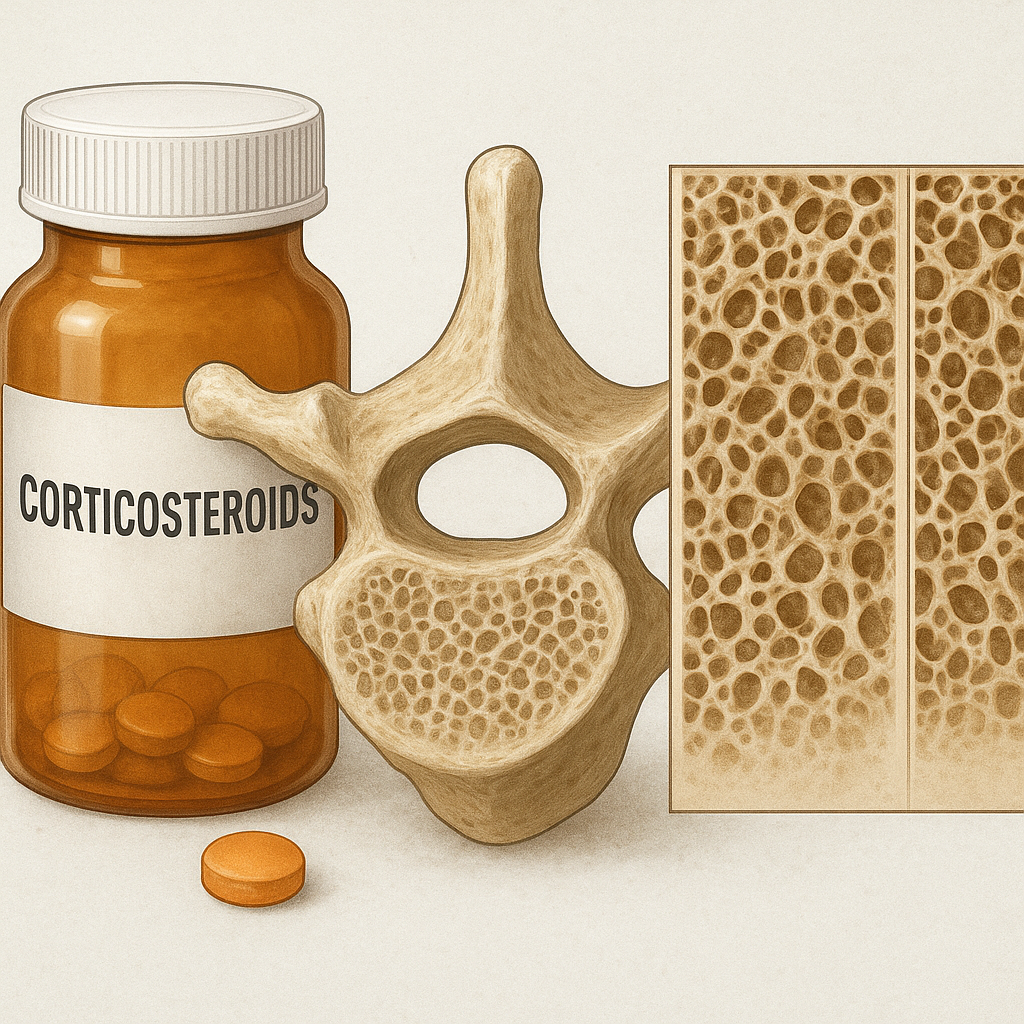
- Medication Management: For those at high risk of osteoporosis, healthcare providers may consider prescribing medications that help strengthen bones, such as bisphosphonates or other osteoporosis treatments.
- Regular Monitoring: Routine check-ups and bone density screenings can help monitor bone health and identify any changes early on.
Conclusion
The link between bone health and chronic illnesses like diabetes is a critical area of research and clinical practice. As the prevalence of diabetes continues to rise, understanding its impact on bone health becomes increasingly important. By recognizing the mechanisms through which diabetes affects bone density and implementing effective strategies for prevention and management, healthcare providers can significantly improve the quality of life for individuals living with diabetes. Ultimately, a holistic approach that addresses both metabolic health and bone health is essential for promoting overall well-being in patients with chronic illnesses.