Bone remodeling is a vital biological process that ensures the maintenance, repair, and adaptation of the skeletal system throughout an individual’s life. This dynamic process involves the continuous resorption of old bone tissue and the formation of new bone, allowing the skeleton to respond to various physiological demands and mechanical stresses. Understanding bone remodeling is crucial for comprehending how bones maintain their strength and integrity, as well as how various factors can influence this process, leading to conditions such as osteoporosis and other bone-related diseases.
The Mechanisms of Bone Remodeling
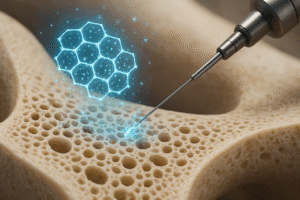
Bone remodeling is a complex interplay between two primary cell types: osteoclasts and osteoblasts. Osteoclasts are responsible for the resorption of bone, breaking down the mineralized matrix and releasing calcium and other minerals into the bloodstream. In contrast, osteoblasts are involved in the formation of new bone, synthesizing the organic components of the bone matrix and facilitating the mineralization process. This balance between resorption and formation is crucial for maintaining bone density and overall skeletal health.
The Role of Osteoclasts
Osteoclasts originate from monocyte/macrophage lineage and are characterized by their large size and multinucleated structure. These cells are activated in response to various signals, including hormones such as parathyroid hormone (PTH) and calcitonin, as well as local factors like RANKL (Receptor Activator of Nuclear Factor Kappa-Β Ligand). Once activated, osteoclasts adhere to the bone surface and create a sealed microenvironment where they secrete acids and proteolytic enzymes. This process dissolves the mineral component of bone and degrades the organic matrix, leading to the release of calcium and phosphate into the circulation.
The Role of Osteoblasts
Osteoblasts, on the other hand, are derived from mesenchymal stem cells and play a crucial role in bone formation. These cells synthesize collagen and other proteins that form the organic matrix of bone, known as osteoid. Once the osteoid is laid down, osteoblasts facilitate the mineralization process by promoting the deposition of calcium phosphate crystals. As osteoblasts become embedded in the matrix they produce, they differentiate into osteocytes, which are mature bone cells that help regulate the bone remodeling process by communicating with other bone cells and sensing mechanical strain.
Factors Influencing Bone Remodeling
Bone remodeling is influenced by a variety of factors, including hormonal regulation, mechanical loading, nutritional status, and age. Understanding these factors is essential for developing strategies to promote bone health and prevent bone-related diseases.
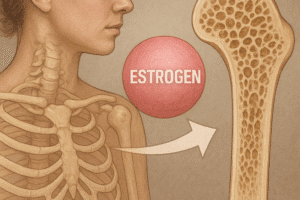
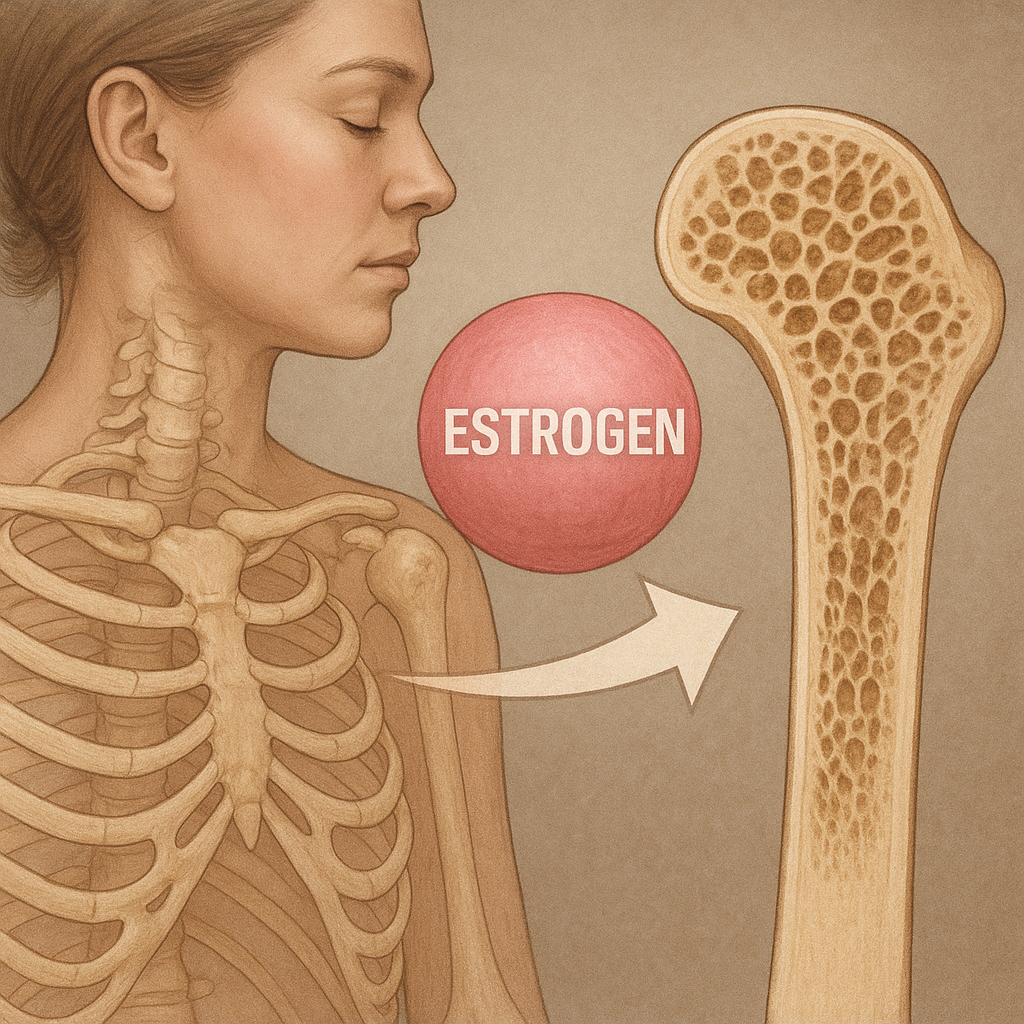
Hormonal Regulation
Hormones play a significant role in regulating bone remodeling. Estrogen, for example, is known to inhibit osteoclast activity, thereby reducing bone resorption. This is one reason why postmenopausal women, who experience a decline in estrogen levels, are at a higher risk for osteoporosis. Similarly, testosterone has been shown to promote bone formation and inhibit bone resorption, highlighting the importance of sex hormones in maintaining bone density.
Mechanical Loading
The mechanical forces exerted on bones during physical activity are crucial for stimulating bone remodeling. Weight-bearing exercises, such as running or resistance training, promote bone formation by increasing the activity of osteoblasts. Conversely, a sedentary lifestyle can lead to decreased bone density, as the lack of mechanical stress results in reduced stimulation of bone formation and increased resorption. This mechanotransduction process is essential for adapting bone structure to meet the demands of physical activity.
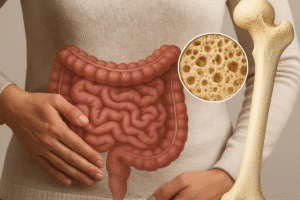
Nutritional Status
Nutrition also plays a critical role in bone health. Adequate intake of calcium and vitamin D is essential for maintaining bone density and supporting the remodeling process. Calcium is a key component of the bone matrix, while vitamin D is necessary for calcium absorption in the intestines. Deficiencies in these nutrients can lead to impaired bone remodeling and increased risk of fractures. Additionally, other nutrients such as magnesium, phosphorus, and vitamin K also contribute to bone health and should not be overlooked.
Age and Bone Remodeling
As individuals age, the balance between bone resorption and formation tends to shift, often leading to a net loss of bone mass. This is particularly evident in postmenopausal women due to the decline in estrogen levels. In older adults, osteoblast activity decreases, while osteoclast activity may remain unchanged or even increase, resulting in a higher risk of osteoporosis and fractures. Understanding the age-related changes in bone remodeling is crucial for developing effective prevention and treatment strategies for age-related bone loss.
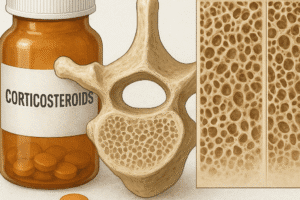
Bone Remodeling and Disease
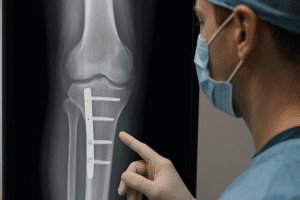
Disruptions in the bone remodeling process can lead to various bone diseases, with osteoporosis being one of the most common. Osteoporosis is characterized by decreased bone density and increased fragility, making individuals more susceptible to fractures. Other conditions, such as Paget’s disease of bone, osteomalacia, and hyperparathyroidism, also involve alterations in the remodeling process and can have significant impacts on bone health.
Osteoporosis
Osteoporosis is often referred to as a “silent disease” because it can progress without noticeable symptoms until a fracture occurs. The condition is primarily caused by an imbalance between bone resorption and formation, leading to a decrease in bone mass and structural integrity. Risk factors for osteoporosis include age, gender, family history, low body weight, and lifestyle factors such as smoking and excessive alcohol consumption. Preventive measures, including adequate nutrition, regular exercise, and, in some cases, medication, are essential for reducing the risk of osteoporosis.
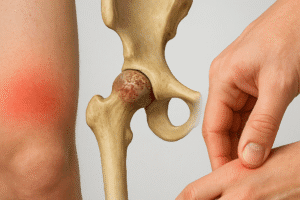
Paget’s Disease of Bone
Paget’s disease is a chronic disorder characterized by abnormal bone remodeling, leading to enlarged and weakened bones. The exact cause of Paget’s disease is not fully understood, but it is believed to involve a combination of genetic and environmental factors. Individuals with Paget’s disease may experience bone pain, deformities, and an increased risk of fractures. Treatment options include medications that inhibit osteoclast activity and promote normal bone remodeling.
Osteomalacia
Osteomalacia is a condition characterized by the softening of bones due to inadequate mineralization, often resulting from vitamin D deficiency. This condition can lead to bone pain, muscle weakness, and an increased risk of fractures. Treatment typically involves addressing the underlying nutritional deficiencies and may include vitamin D and calcium supplementation.
Conclusion
Bone remodeling is a complex and dynamic process that plays a crucial role in maintaining skeletal health. Understanding the mechanisms involved in bone remodeling, as well as the factors that influence this process, is essential for promoting bone health and preventing bone-related diseases. As research continues to uncover the intricacies of bone biology, it is hoped that new therapeutic strategies will emerge to address the challenges posed by conditions such as osteoporosis and other disorders of bone remodeling. By prioritizing nutrition, physical activity, and hormonal balance, individuals can take proactive steps to support their bone health throughout their lives.