The phenomenon of bones breaking more easily in the elderly is a significant concern in the field of geriatric health. As individuals age, their bodies undergo various changes that can lead to an increased risk of fractures. Understanding the underlying reasons for this vulnerability is crucial for developing effective prevention strategies and improving the quality of life for older adults. This article will explore the biological, lifestyle, and environmental factors that contribute to the increased fragility of bones in the elderly, as well as potential measures to mitigate these risks.
Biological Factors Contributing to Bone Fragility
One of the primary reasons bones become more susceptible to fractures in older adults is the natural aging process. As people age, several biological changes occur that directly affect bone density and strength.
Bone Density and Osteoporosis
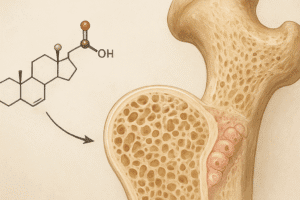
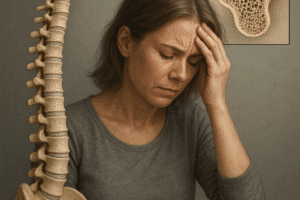
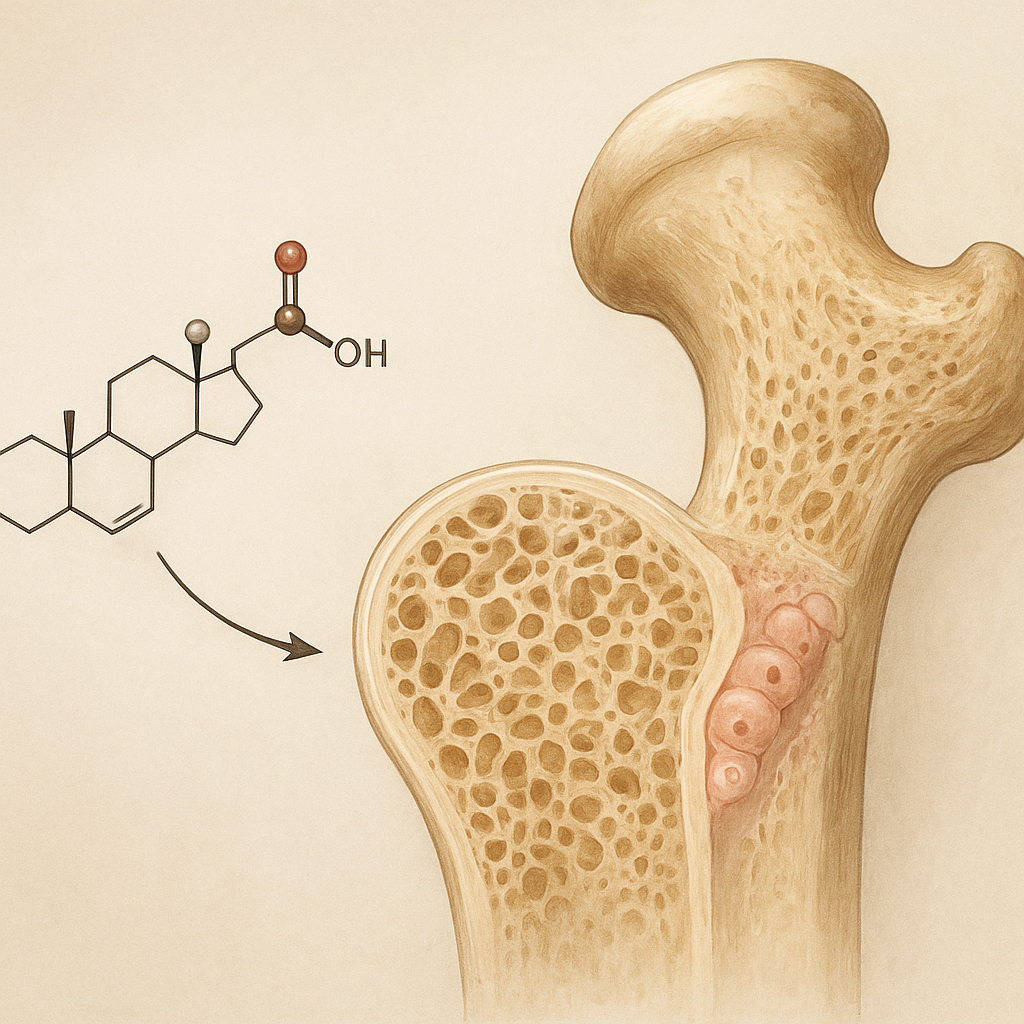
Bone density refers to the amount of bone mineral in a given volume of bone. It is a critical factor in determining the strength and resilience of bones. In elderly individuals, bone density tends to decrease due to a condition known as osteoporosis. Osteoporosis is characterized by a reduction in bone mass and deterioration of bone tissue, leading to an increased risk of fractures.
- Hormonal Changes: One of the significant contributors to osteoporosis in older adults is hormonal changes, particularly in women after menopause. The decline in estrogen levels significantly impacts bone density, as estrogen plays a vital role in maintaining bone health.
- Calcium and Vitamin D Deficiency: Aging can also lead to decreased absorption of calcium and vitamin D, essential nutrients for bone health. A deficiency in these nutrients can further exacerbate bone loss.
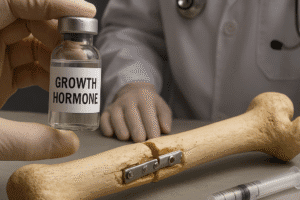
- Bone Remodeling: The process of bone remodeling, which involves the resorption of old bone and the formation of new bone, becomes less efficient with age. This imbalance can lead to a net loss of bone mass over time.
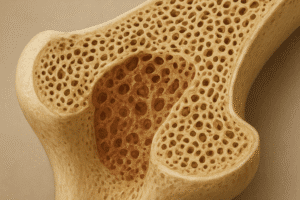
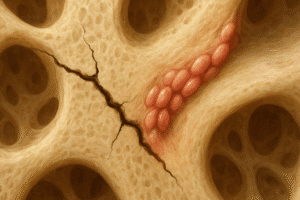
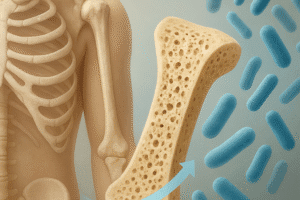
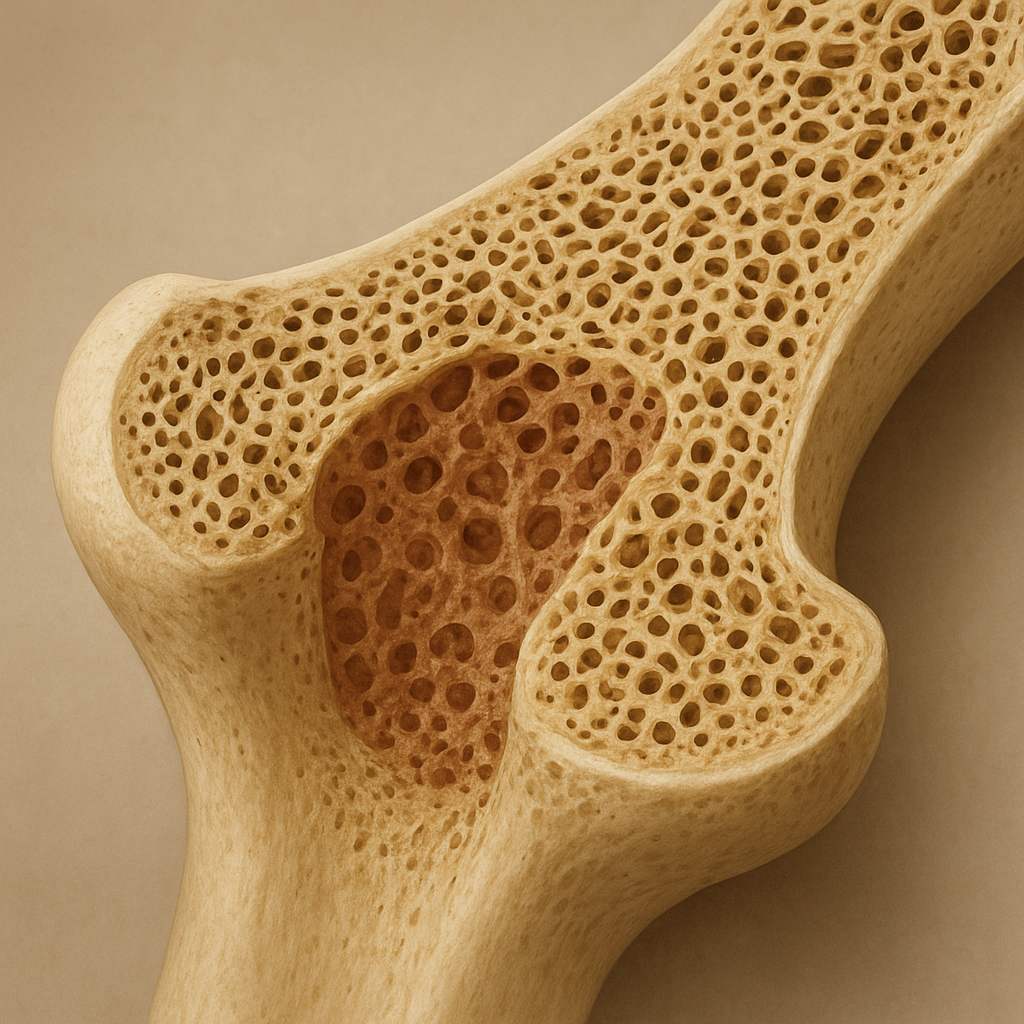
Changes in Bone Structure
In addition to changes in bone density, the microarchitecture of bones also deteriorates with age. The trabecular bone, which is the spongy tissue inside bones, becomes less dense and more porous, making it more prone to fractures. This structural change can significantly weaken the overall integrity of bones, increasing the likelihood of breaks even with minor falls or injuries.
Lifestyle Factors Affecting Bone Health
While biological factors play a significant role in bone fragility, lifestyle choices also contribute to the risk of fractures in the elderly. Understanding these factors can help in developing strategies to promote better bone health.
Physical Activity
Regular physical activity is essential for maintaining bone strength. Weight-bearing exercises, in particular, stimulate bone formation and help preserve bone density. However, many elderly individuals lead sedentary lifestyles due to various reasons, including mobility issues, fear of falling, or lack of motivation.
- Impact of Sedentary Lifestyle: A sedentary lifestyle can lead to muscle weakness and decreased balance, increasing the risk of falls and subsequent fractures. Encouraging older adults to engage in regular physical activity can significantly improve their bone health.
- Types of Exercise: Activities such as walking, dancing, and resistance training can be particularly beneficial for maintaining bone density. Additionally, exercises that improve balance and coordination, such as tai chi, can help prevent falls.
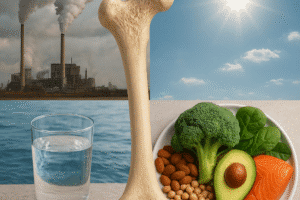
Nutrition and Diet
Nutrition plays a crucial role in bone health. A diet rich in calcium and vitamin D is essential for maintaining bone density. However, many elderly individuals may not consume adequate amounts of these nutrients due to various factors, including changes in appetite, difficulty in preparing meals, or financial constraints.
- Calcium Sources: Dairy products, leafy greens, and fortified foods are excellent sources of calcium. Ensuring that older adults have access to these foods can help improve their bone health.
- Vitamin D Sources: Vitamin D can be obtained through sunlight exposure and certain foods, such as fatty fish and fortified products. However, older adults may have limited sun exposure due to mobility issues or skin sensitivity, making supplementation necessary in some cases.
Medication and Health Conditions
Certain medications and health conditions can also impact bone health in the elderly. For instance, long-term use of corticosteroids can lead to bone loss, while conditions such as rheumatoid arthritis and hyperthyroidism can further exacerbate the risk of fractures.
- Medication Management: It is essential for healthcare providers to regularly review the medications of elderly patients to identify any that may negatively affect bone health. Adjusting medications or implementing preventive measures can help mitigate these risks.
- Chronic Health Conditions: Managing chronic health conditions effectively can also play a role in maintaining bone health. Regular check-ups and a comprehensive treatment plan can help reduce the risk of fractures.
Environmental Factors and Fall Risks
Environmental factors also contribute significantly to the risk of fractures in the elderly. The likelihood of falls increases with age, and falls are a leading cause of fractures among older adults.
Home Safety
Many falls occur in the home environment, where hazards may be present. Simple modifications can significantly reduce the risk of falls and, consequently, fractures.
- Removing Hazards: Clutter, loose rugs, and poor lighting can create dangerous conditions for older adults. Ensuring that living spaces are free of obstacles and well-lit can help prevent falls.
- Assistive Devices: The use of assistive devices, such as canes or walkers, can provide additional support and stability for elderly individuals, reducing their risk of falling.
Community and Social Support
Social isolation can also contribute to a higher risk of falls and fractures. Engaging with the community and maintaining social connections can encourage older adults to remain active and seek help when needed.
- Community Programs: Many communities offer programs designed to promote physical activity among older adults. Participating in these programs can help improve strength, balance, and overall well-being.
- Support Networks: Encouraging family and friends to check in on elderly individuals can provide them with the support they need to maintain their independence and safety.
Preventive Measures and Conclusion
Given the various factors contributing to the increased risk of fractures in the elderly, it is essential to implement preventive measures to promote bone health and reduce the likelihood of falls.
Regular Health Screenings
Regular health screenings can help identify individuals at risk for osteoporosis and other conditions that may affect bone health. Early intervention can lead to better outcomes and reduce the risk of fractures.
Education and Awareness
Educating older adults and their caregivers about the importance of bone health, nutrition, and fall prevention strategies is crucial. Awareness can empower individuals to take proactive steps in maintaining their bone health.
Conclusion
In conclusion, the increased fragility of bones in the elderly is a multifaceted issue influenced by biological, lifestyle, and environmental factors. By understanding these factors and implementing preventive measures, we can help reduce the risk of fractures and improve the overall quality of life for older adults. Promoting bone health through education, physical activity, and community support is essential in addressing this significant health concern.