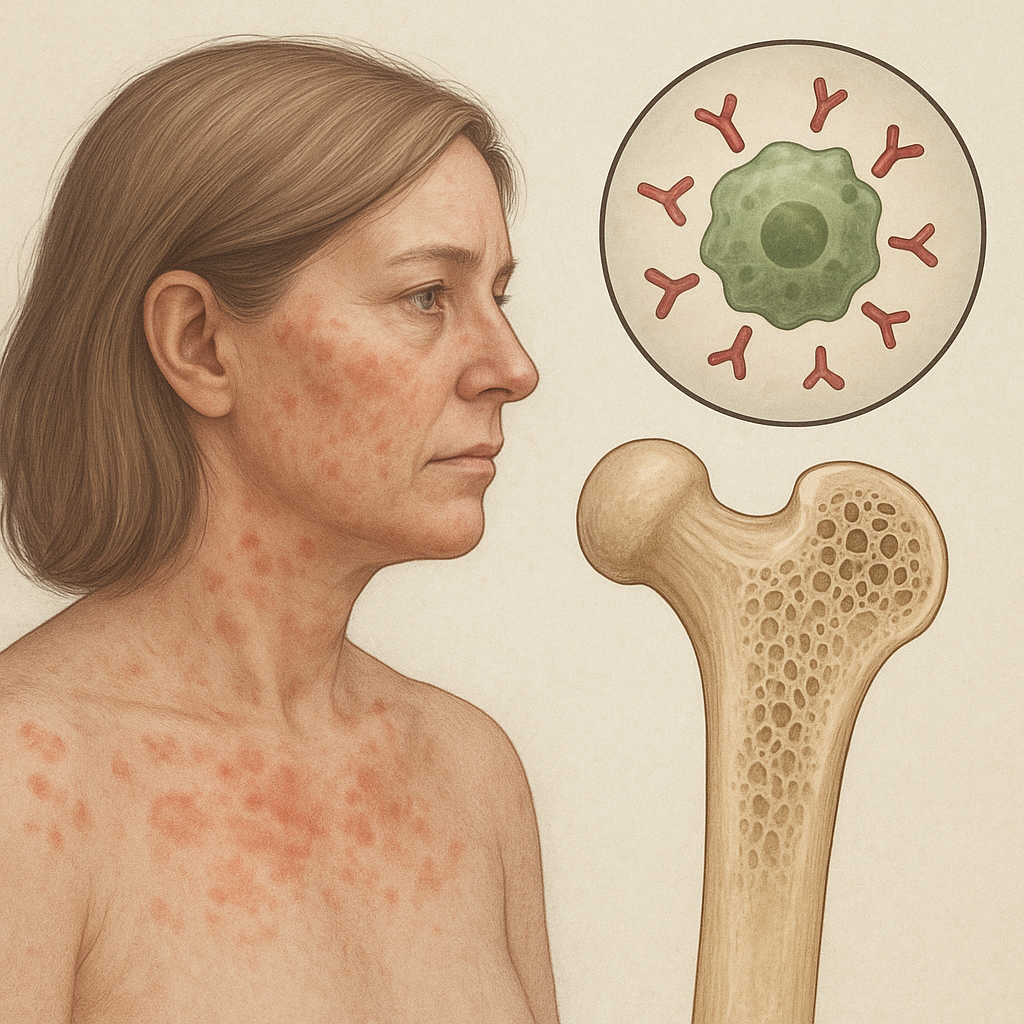
The complex interplay between the immune system and the skeletal framework has garnered growing attention in recent years. Emerging evidence highlights how dysregulated immune responses can drive excessive bone breakdown, leading to compromised skeletal integrity. Understanding the mechanisms behind this connection is essential for designing targeted interventions that preserve bone health in patients with immune-mediated disorders.
Pathways Linking Immune Dysregulation and Bone Resorption
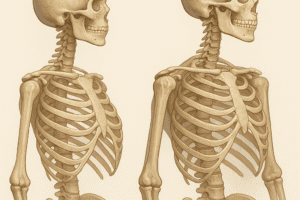
Bone remodeling is a dynamic process orchestrated by osteoblasts (bone-forming cells) and osteoclasts (bone-resorbing cells). Under normal conditions, these activities remain balanced, ensuring continuous renewal and mineral homeostasis. However, in the context of autoimmune diseases, the equilibrium is disrupted by chronic inflammation and aberrant cytokine production. Pro-inflammatory mediators such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6) and interleukin-17 (IL-17) stimulate osteoclastogenesis, tipping the scale toward net bone loss.
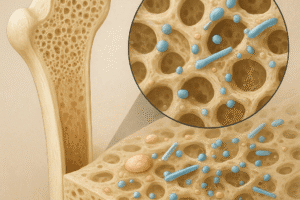
Key molecular players include the receptor activator of nuclear factor kappa-B ligand (RANKL) and its decoy receptor osteoprotegerin (OPG). Activated T cells and synovial fibroblasts in autoimmune settings express elevated levels of RANKL, promoting osteoclast differentiation. Concurrently, OPG production may be suppressed, further enhancing osteoclastic activity. This process is often accompanied by increased production of matrix metalloproteinases (MMPs) that degrade the bone matrix.
Immune Cell Contributions
- Th17 cells: Secrete IL-17 to potentiate RANKL expression.
- Macrophages: Release TNF-α and IL-1β, enhancing osteoclast survival.
- B cells: Can produce RANKL and autoantibodies that aggravate inflammation.
Clinical Manifestations and Risk Assessment
Patients with systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), inflammatory bowel disease (IBD) and other autoimmune conditions exhibit higher rates of low bone mineral density (BMD) and osteoporosis. Epidemiological studies reveal that fracture risk in RA patients, for instance, can be up to three times greater than in age-matched controls. Factors contributing to this increased vulnerability include prolonged disease activity, glucocorticoid therapy, reduced mobility and nutritional deficiencies.
Assessing bone health in immune-mediated disorders requires a multifaceted approach:
- Dual-energy X-ray absorptiometry (DXA) scans for BMD measurement.
- Biochemical markers of bone turnover, such as serum C-terminal telopeptide (CTX) and bone-specific alkaline phosphatase (BSAP).
- Inflammatory indices, including C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), to correlate disease activity with bone loss.
- Risk factor evaluation: age, gender, family history, medication profile and lifestyle habits.
Early identification of high-risk individuals allows for timely intervention, potentially preventing debilitating fractures and preserving quality of life.
Therapeutic Strategies to Mitigate Bone Loss
Addressing bone loss in patients with autoimmune diseases demands an integrated strategy that targets both immune dysfunction and skeletal integrity. Core objectives include reducing inflammatory burden, inhibiting osteoclast activity and enhancing osteoblast function.
Immunomodulatory Approaches
- Biologic agents such as anti-TNF-α and anti-IL-6 receptor antibodies diminish pro-osteoclastogenic signals.
- Janus kinase (JAK) inhibitors block intracellular pathways driving cytokine production.
- Low-dose methotrexate and other conventional disease-modifying antirheumatic drugs (DMARDs) can decrease systemic inflammation and associated bone damage.
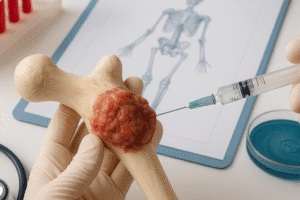
Bone-Targeted Therapies
- Bisphosphonates: Inhibit osteoclast-mediated bone resorption by disrupting the mevalonate pathway.
- Denosumab: A monoclonal antibody against RANKL, directly preventing osteoclast differentiation.
- Selective estrogen receptor modulators (SERMs): Provide anabolic effects on bone in postmenopausal women with autoimmune diseases.
- Parathyroid hormone analogs: Stimulate osteoblastic activity when used intermittently.
Lifestyle modifications—such as weight-bearing exercise, smoking cessation and adequate intake of calcium and vitamin D—serve as adjunctive measures. Regular monitoring ensures optimal dosing and helps detect potential adverse events, such as osteonecrosis of the jaw with certain high-potency antiresorptives.
Emerging Research and Future Directions
Ongoing investigations aim to unravel novel molecular pathways linking immunity and skeletal health. Recent studies highlight the role of the gut microbiome in modulating systemic inflammation and bone metabolism. Manipulating microbial composition through prebiotics, probiotics or fecal microbiota transplantation offers a promising frontier for skeletal protection.
Advanced imaging modalities—such as high-resolution peripheral quantitative computed tomography (HR-pQCT)—are improving our ability to detect microarchitectural bone changes before significant BMD loss occurs. Additionally, biomarkers derived from next-generation sequencing and proteomic profiling may enable personalized risk stratification and targeted intervention.
Gene editing technologies, notably CRISPR-Cas9, hold potential for correcting genetic susceptibilities in autoimmune disorders, thereby reducing secondary bone complications. Research into small-molecule inhibitors that selectively block osteoclast-specific signaling cascades without broad immunosuppression is another exciting avenue.
Through a combination of immunological insights, advanced diagnostics and innovative therapeutics, the goal of preserving bone health in autoimmune disease patients becomes increasingly attainable. Multidisciplinary collaboration among rheumatologists, endocrinologists and immunologists will be critical to translate benchside discoveries into bedside solutions.