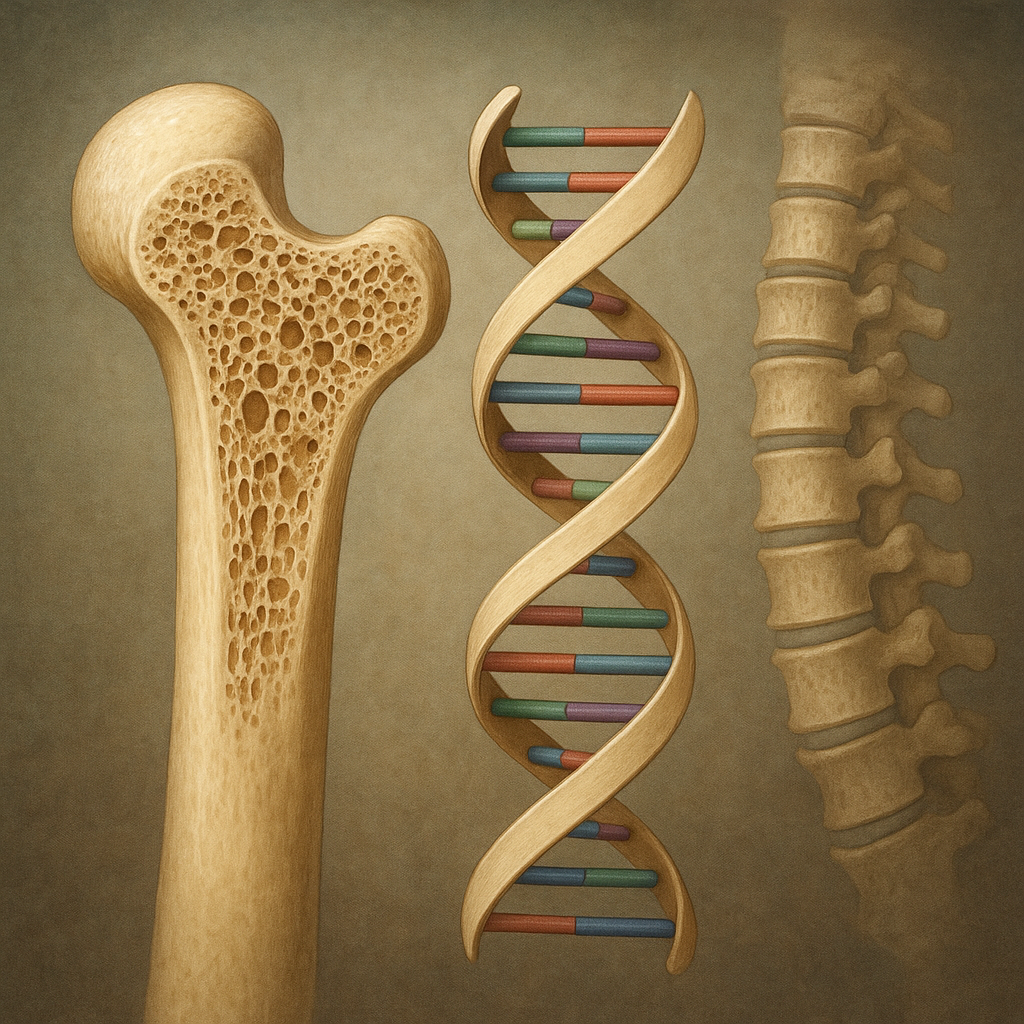
The interplay between **genes** and bone tissue determines individual susceptibility to changes in **bone density**, shaping long-term skeletal health. Recent advances in molecular biology, population studies, and functional genomics have shed light on how specific **polymorphisms**, rare mutations, and regulatory elements orchestrate the complex process of bone formation, maintenance, and repair. Understanding these genetic contributions is vital for developing targeted interventions against **osteoporosis**, **fragility fractures**, and other skeletal disorders.
Genetic Architecture of Bone Density
Heritability and Genome-Wide Studies
Bone Mineral Density (BMD) is a highly heritable trait, with twin and family studies estimating that up to 80% of the variation in BMD is genetically determined. Large-scale **GWAS** (Genome-Wide Association Studies) have identified hundreds of loci associated with BMD measurements at the lumbar spine, femoral neck, and total hip. Many of these loci reside near genes involved in bone metabolism and remodeling, illustrating a polygenic nature that involves common **alleles** exerting modest effects.
Rare Variants versus Common Polymorphisms
While many common **polymorphisms** contribute small increments to BMD, rare coding variants can have large phenotypic consequences. Exome sequencing in families with extreme bone phenotypes has uncovered mutations in genes such as SOST (sclerostin), which leads to high bone mass when inactivated, and LRP5, a co-receptor in the **Wnt signaling** pathway essential for osteoblast function. Such discoveries highlight pathways that can be harnessed therapeutically.
Major Genetic Variants and Pathways
Wnt/β-Catenin Signaling
The **Wnt signaling** cascade is central to osteoblast proliferation and maturation. Variants in genes encoding Wnt ligands, receptors (LRP5, LRP6), and inhibitors (SOST, DKK1) modulate bone formation. Loss-of-function mutations in **LRP5** reduce bone accrual, predisposing carriers to **osteoporosis**, whereas inactivating mutations in **SOST** result in sclerosing bone dysplasias characterized by excessive bone mass.
RANK–RANKL–OPG Axis
Bone resorption is regulated by the interaction between Receptor Activator of Nuclear Factor κB Ligand (RANKL) and its receptor RANK, with Osteoprotegerin (OPG) acting as a decoy. Mutations that enhance RANKL expression or diminish OPG activity tip the balance toward osteoclast activation, increasing bone turnover and fragility. Understanding variants in the receptor activator of nuclear factor kappa-B ligand pathway has led to biologics that block RANKL and reduce fracture risk.
Collagen and Extracellular Matrix
Type I **collagen** is the primary structural protein in bone. Dominant-negative mutations in COL1A1 and COL1A2 genes cause Osteogenesis Imperfecta (OI), characterized by brittle bones, blue sclera, and dentinogenesis imperfecta. Beyond OI, milder allelic variants can subtly weaken the matrix, contributing to age-related bone loss. Research into post-translational modifications of collagen is uncovering additional genetic regulators of matrix quality.
Bone Fragility Syndromes: Monogenic Disorders
Osteogenesis Imperfecta
OI represents a classic monogenic disorder of bone fragility. Over 90% of cases are due to dominant mutations in COL1A1 or COL1A2, but recessive forms involve genes responsible for collagen folding, post-translational hydroxylation, and triple-helix stabilization. Phenotypes range from perinatal lethality to mild adult-onset fractures. Advances in next-generation sequencing have expedited diagnosis and enabled genotype-guided management.
Hypophosphatasia and Mineralization Defects
Mutations in ALPL, encoding tissue-nonspecific alkaline phosphatase, cause Hypophosphatasia, marked by defective mineralization of bone and teeth. Severity correlates with residual enzyme activity. Genetic insights have led to enzyme replacement therapy that dramatically improves skeletal outcomes in severe infantile forms.
Other Rare Syndromes
- Marfan syndrome: FBN1 mutations affect connective tissue integrity, indirectly impacting bone architecture.
- Stickler syndrome: COL2A1 defects alter cartilage and subchondral bone health.
- Cleidocranial dysplasia: RUNX2 haploinsufficiency impairs osteoblast differentiation and skull ossification.
Clinical Implications and Therapeutic Strategies
Genetic Screening and Risk Prediction
Polygenic risk scores (PRS) aggregate the effect of multiple BMD-associated variants to predict individual fracture risk. Integrating PRS with clinical risk factors such as age, sex, and lifestyle generates more accurate stratification than traditional models alone. Early identification of high-risk individuals allows prompt initiation of preventive measures.
Targeted Biologics and Small Molecules
Genetic discoveries have directly informed drug development. Monoclonal antibodies against SOST (romosozumab) stimulate bone formation, while RANKL inhibitors (denosumab) suppress osteoclast activity. Small molecules modulating the **vitamin D receptor** pathway enhance mineral homeostasis. Personalized therapy selection based on genetic profile optimizes efficacy and minimizes adverse effects.
Gene Editing and Future Interventions
CRISPR/Cas9 technology offers potential cures for monogenic bone diseases by correcting pathogenic mutations in patient-derived stem cells. Preclinical models have demonstrated successful restoration of normal bone matrix production in cells harboring COL1A1 mutations. Ethical considerations and delivery challenges remain before these techniques can transition to the clinic.
Future Directions in Bone Genetics Research
Epigenetic Regulation
DNA methylation, histone modifications, and non-coding RNAs fine-tune gene expression in bone cells. Profiling the **epigenome** of osteoblasts and osteoclasts under physiological and pathological conditions will uncover new therapeutic targets that restore healthy bone remodeling.
Single-Cell Genomics
Single-cell RNA sequencing is dissecting the heterogeneity of bone marrow niches, revealing subpopulations of progenitor cells with distinct osteogenic potential. Mapping gene expression at this resolution will illuminate how rare cell types contribute to skeletal maintenance and repair.
Systems Biology Approaches
Integrative models combining genomic, transcriptomic, proteomic, and metabolomic data aim to reconstruct the regulatory networks that govern bone homeostasis. Such holistic frameworks will predict system responses to genetic perturbations and pharmacological interventions with unprecedented accuracy.