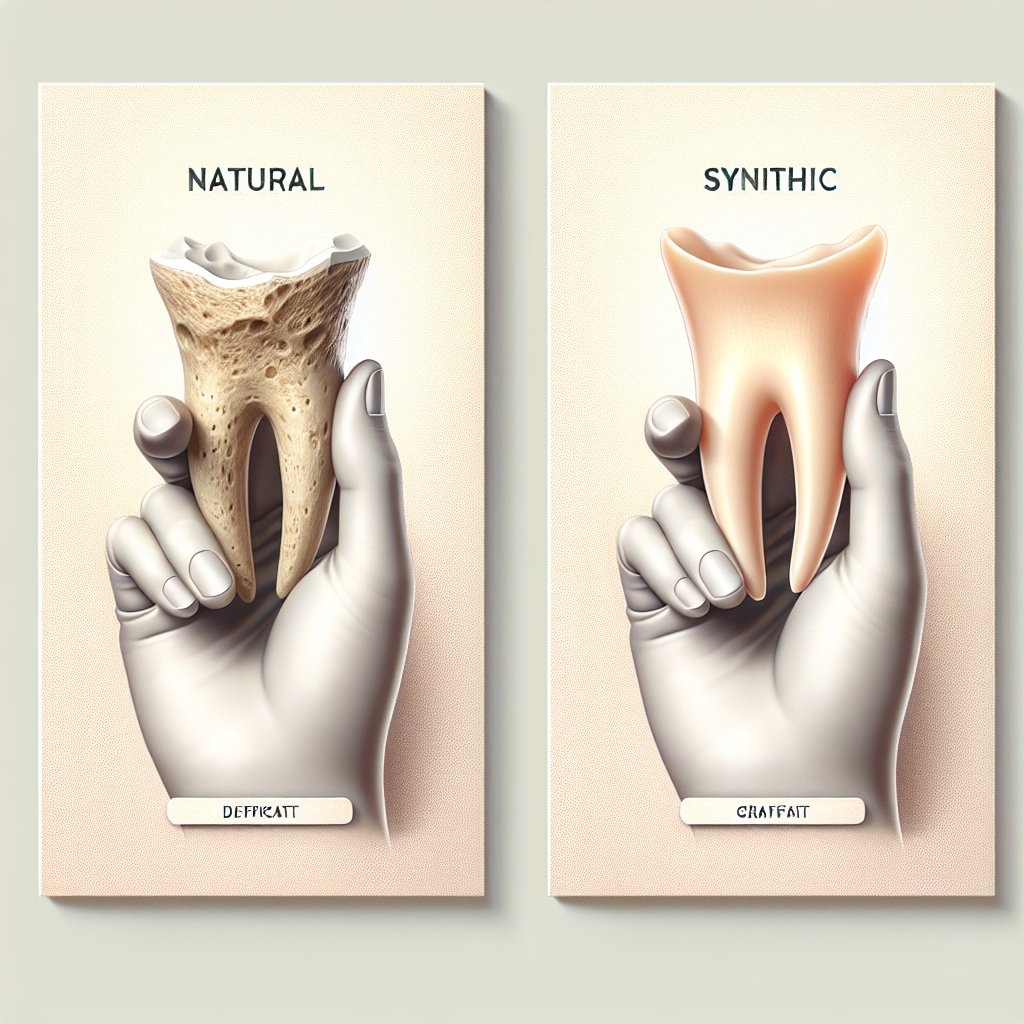
The difference between natural and synthetic bone grafts is a crucial topic in the field of orthopedic surgery and regenerative medicine. As the demand for effective treatments for bone defects and injuries continues to rise, understanding the distinctions between these two types of grafts becomes essential for both medical professionals and patients. This article will explore the characteristics, advantages, and disadvantages of natural and synthetic bone grafts, as well as their applications in clinical practice.
Understanding Natural Bone Grafts
Natural bone grafts, often referred to as autografts or allografts, are derived from biological sources. Autografts are harvested from the patient’s own body, typically from areas such as the iliac crest, while allografts are obtained from cadaveric donors. These grafts are used to promote bone healing and regeneration in various orthopedic procedures.
Types of Natural Bone Grafts
- Autografts: These are the gold standard in bone grafting. Since they come from the same individual, there is a lower risk of rejection and disease transmission. Autografts contain living cells and growth factors that enhance the healing process.
- Allografts: These grafts are sourced from deceased donors and are processed to ensure safety and sterility. Allografts can be used in larger quantities and are beneficial when extensive bone reconstruction is needed.
Advantages of Natural Bone Grafts
Natural bone grafts offer several advantages:
- Biocompatibility: Being derived from biological sources, natural grafts are highly compatible with the human body, reducing the risk of rejection.
- Osteoconductivity: Natural grafts provide a scaffold for new bone growth, allowing for the integration of host bone with the graft.
- Presence of Growth Factors: Autografts, in particular, contain growth factors that stimulate bone healing and regeneration.
Disadvantages of Natural Bone Grafts
Despite their benefits, natural bone grafts also have some drawbacks:
- Harvesting Complications: Autografts require a second surgical site, which can lead to complications such as infection, pain, and longer recovery times.
- Limited Availability: Allografts may not always be available in the required size or shape, and there is a risk of disease transmission, although this is minimized through rigorous screening.
Exploring Synthetic Bone Grafts
Synthetic bone grafts are man-made materials designed to mimic the properties of natural bone. They are often composed of biocompatible materials such as ceramics, polymers, or composites. Synthetic grafts have gained popularity due to their versatility and the ability to overcome some limitations associated with natural grafts.
Types of Synthetic Bone Grafts
- Calcium Phosphate Ceramics: These materials closely resemble the mineral component of bone and promote osteoconductivity. They are commonly used in various orthopedic applications.
- Bioactive Glass: This type of synthetic graft can bond with bone and stimulate cellular activity, making it an effective option for bone regeneration.
- Polymers: Biodegradable polymers can be used to create scaffolds that support bone growth while gradually degrading over time.
Advantages of Synthetic Bone Grafts
Synthetic bone grafts offer several benefits:
- Availability: Synthetic grafts can be produced in large quantities and tailored to specific shapes and sizes, ensuring that surgeons have the materials they need for various procedures.
- No Donor Site Morbidity: Since synthetic grafts do not require harvesting from the patient, there is no risk of complications associated with a second surgical site.
- Controlled Composition: The properties of synthetic grafts can be engineered to enhance specific characteristics, such as porosity and mechanical strength.
Disadvantages of Synthetic Bone Grafts
However, synthetic bone grafts also have limitations:
- Biological Integration: While synthetic grafts can provide a scaffold for bone growth, they may not integrate as effectively with the host bone compared to natural grafts.
- Absence of Living Cells: Most synthetic grafts lack the living cells and growth factors found in natural grafts, which can limit their effectiveness in promoting bone healing.
Clinical Applications and Considerations
The choice between natural and synthetic bone grafts often depends on the specific clinical scenario, the patient’s needs, and the surgeon’s preferences. Both types of grafts have their place in orthopedic surgery, and understanding their differences can help guide treatment decisions.
Indications for Natural Bone Grafts
Natural bone grafts are often indicated in the following situations:
- Complex Fractures: In cases of severe fractures where bone healing is compromised, autografts can provide the necessary biological support for healing.
- Bone Defects: Natural grafts are commonly used in reconstructive surgeries to fill large bone defects resulting from trauma or tumor resection.
- Spinal Fusion: Autografts are frequently used in spinal fusion procedures to promote the fusion of vertebrae.
Indications for Synthetic Bone Grafts
Synthetic bone grafts are often preferred in the following scenarios:
- Less Invasive Procedures: In minimally invasive surgeries, synthetic grafts can be advantageous due to their ease of use and availability.
- Large-Scale Applications: When large quantities of graft material are needed, synthetic options can be more practical and cost-effective.
- Specific Mechanical Properties: In cases where specific mechanical strength or porosity is required, synthetic grafts can be engineered to meet these needs.
Future Directions in Bone Grafting
The field of bone grafting is continuously evolving, with ongoing research aimed at improving both natural and synthetic grafts. Innovations in tissue engineering, 3D printing, and biomaterials are paving the way for more effective solutions in bone regeneration.
Tissue Engineering and Regenerative Medicine
Tissue engineering combines principles of biology and engineering to create scaffolds that support the growth of new tissue. Researchers are exploring the use of stem cells, growth factors, and bioactive materials to enhance the healing process and improve the integration of grafts with host bone.
3D Printing in Bone Grafting
3D printing technology allows for the creation of customized grafts tailored to the specific anatomical needs of patients. This approach can improve the fit and integration of grafts, potentially leading to better clinical outcomes.
Biomaterials and Smart Grafts
Advancements in biomaterials are leading to the development of “smart” grafts that can respond to the biological environment. These grafts may release growth factors or change their properties in response to physiological conditions, enhancing their effectiveness in promoting bone healing.
Conclusion
In summary, the difference between natural and synthetic bone grafts lies in their sources, properties, and applications. Natural bone grafts offer biological advantages, while synthetic grafts provide versatility and ease of use. The choice between the two depends on various factors, including the specific clinical situation and patient needs. As research continues to advance, the future of bone grafting holds promise for improved outcomes and innovative solutions in orthopedic surgery.