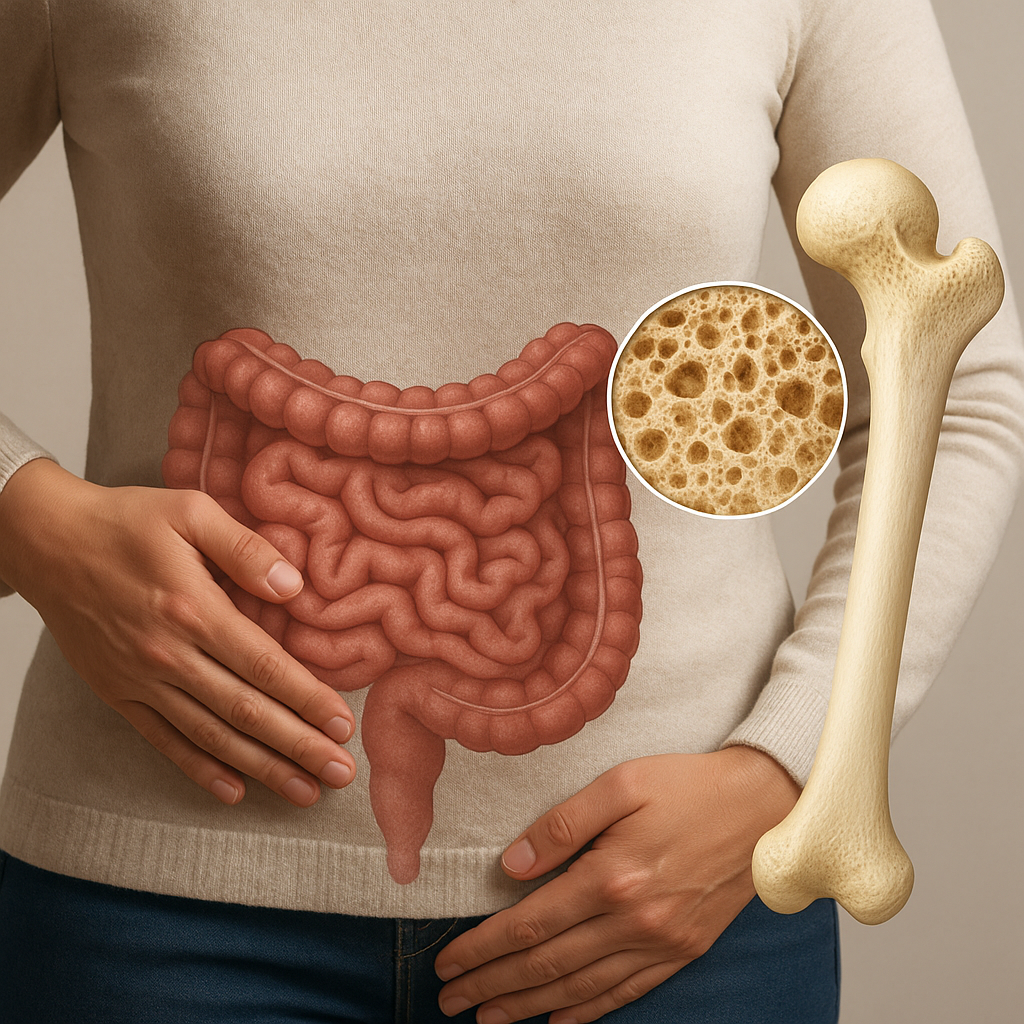
The intricate relationship between the gastrointestinal environment and skeletal integrity has emerged as a vital field of research. Recent discoveries reveal that the gut microbiota profoundly influences bone physiology, shaping processes from mineral absorption to immune regulation. By unraveling this connection, clinicians and researchers can develop novel strategies to enhance bone density, mitigate osteoporosis, and optimize overall musculoskeletal health.
Microbiota and Bone Remodeling
Composition and Diversity of the Gut Ecosystem
The human digestive tract hosts trillions of microorganisms, including bacteria, fungi, and viruses. This complex community maintains a delicate equilibrium that affects systemic health. Dysbiosis—an imbalance in microbial populations—can trigger chronic inflammation and impair nutrient uptake, both of which are detrimental to bone remodeling.
Effects on Osteoblasts and Osteoclasts
Bone remodeling depends on the coordinated activity of osteoblasts (cells that form new bone) and osteoclasts (cells that resorb bone). Gut-derived metabolites, particularly short-chain fatty acids (SCFAs), play a pivotal role in modulating the differentiation and function of these cells. For instance, butyrate enhances osteoblast activity while suppressing excessive osteoclastogenesis, thereby promoting skeletal integrity.
Mechanisms Linking Gut and Bone Health
Optimizing Nutrient Absorption
Efficient uptake of key minerals and vitamins is crucial for maintaining strong bones. The gut microbiome influences:
- Mineral solubilization: Microbes transform dietary compounds into absorbable forms, boosting calcium absorption and phosphate bioavailability.
- Vitamin synthesis: Certain bacteria produce vitamin K2 and B vitamins essential for bone matrix formation and collagen crosslinking.
Immune System Modulation
The gut acts as an immune organ, educating immune cells that circulate to the bone marrow. An imbalanced microbiome can elevate pro-inflammatory cytokines like TNF-α and IL-6, which stimulate osteoclast activity and bone resorption. Conversely, a healthy microbial community fosters regulatory T cells that protect against inflammatory bone loss.
Endocrine Signaling and Hormonal Interplay
Gut microbes produce metabolites that mimic or influence hormones such as serotonin and estrogen. These compounds indirectly regulate bone turnover by affecting hormone receptors on osteoblasts and osteoclasts. For example, microbial modulation of estrogen metabolism may impact postmenopausal osteoporosis risk.
Clinical Evidence and Trials
Accumulating clinical data supports the concept of the Gut-Bone Axis. Key studies include:
- Randomized trials showing that specific probiotics reduce bone loss in postmenopausal women by modulating inflammatory markers.
- Observational research linking low microbial diversity with decreased bone mineral density in elderly cohorts.
- Intervention studies where prebiotic supplementation improved mineral absorption and reduced markers of bone turnover.
- Animal models demonstrating that germ-free mice exhibit impaired skeletal development, which normalizes after microbial colonization.
Nutritional and Therapeutic Approaches
Translating insights into practice involves a combination of diet, supplements, and lifestyle adjustments:
- Probiotics: Strains such as Lactobacillus rhamnosus and Bifidobacterium longum have shown promise in enhancing bone formation and reducing resorption.
- Prebiotics: Inulin, fructooligosaccharides, and resistant starches feed beneficial bacteria, increasing SCFA production and improving nutrients uptake.
- Dietary patterns: A Mediterranean-style diet rich in vegetables, legumes, and fermented foods supports a balanced microbiome and supplies essential minerals.
- Supplementation: Vitamin D, calcium, and magnesium remain cornerstones of bone health, but their efficacy may be amplified in the context of microbial optimization.
- Pharmacological modulation: Emerging therapies target microbial enzymes or metabolic pathways to favor bone-protective profiles.
Future Perspectives and Research Directions
Despite significant advances, several questions remain. Longitudinal human studies are needed to establish causal relationships and to determine optimal microbial compositions for specific populations. Personalized microbiome profiling could enable tailored interventions, maximizing benefits for individuals at risk of fractures or suffering from chronic inflammatory conditions. The integration of multi-omics technologies—metagenomics, metabolomics, and transcriptomics—will provide deeper insights into the molecular dialogue between gut microbes and bone cells, paving the way for innovative nutrients-based and microbial therapies.