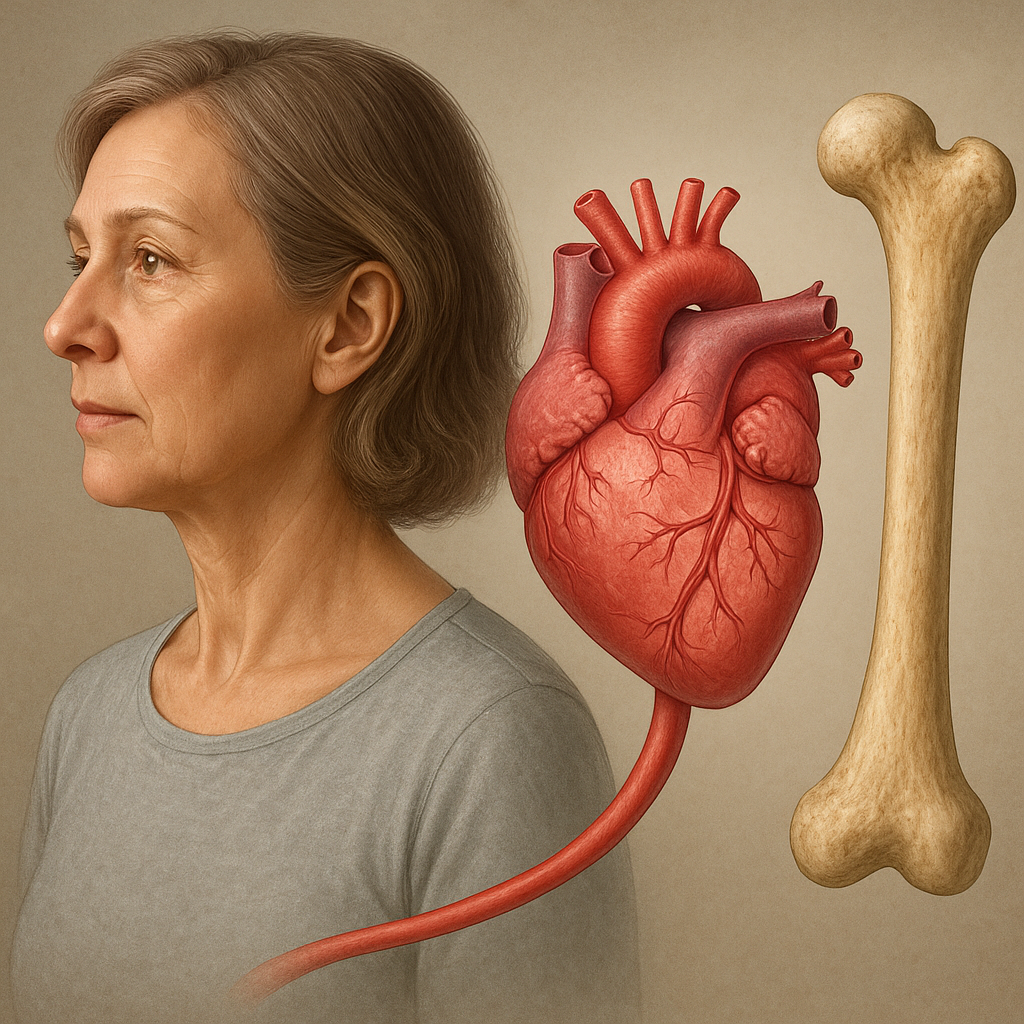
The intricate relationship between skeletal integrity and cardiovascular health has become an area of growing interest among researchers and clinicians. Emerging evidence suggests that parameters traditionally associated with bone quality may also serve as predictors of heart and vessel disease. By unraveling the shared pathways that govern bone turnover and vascular function, medical science is moving closer to integrated strategies in prevention and treatment.
Bone Metabolism and Cardiovascular Interplay
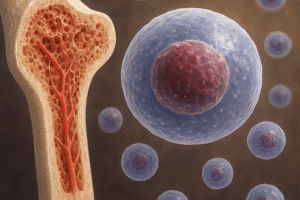
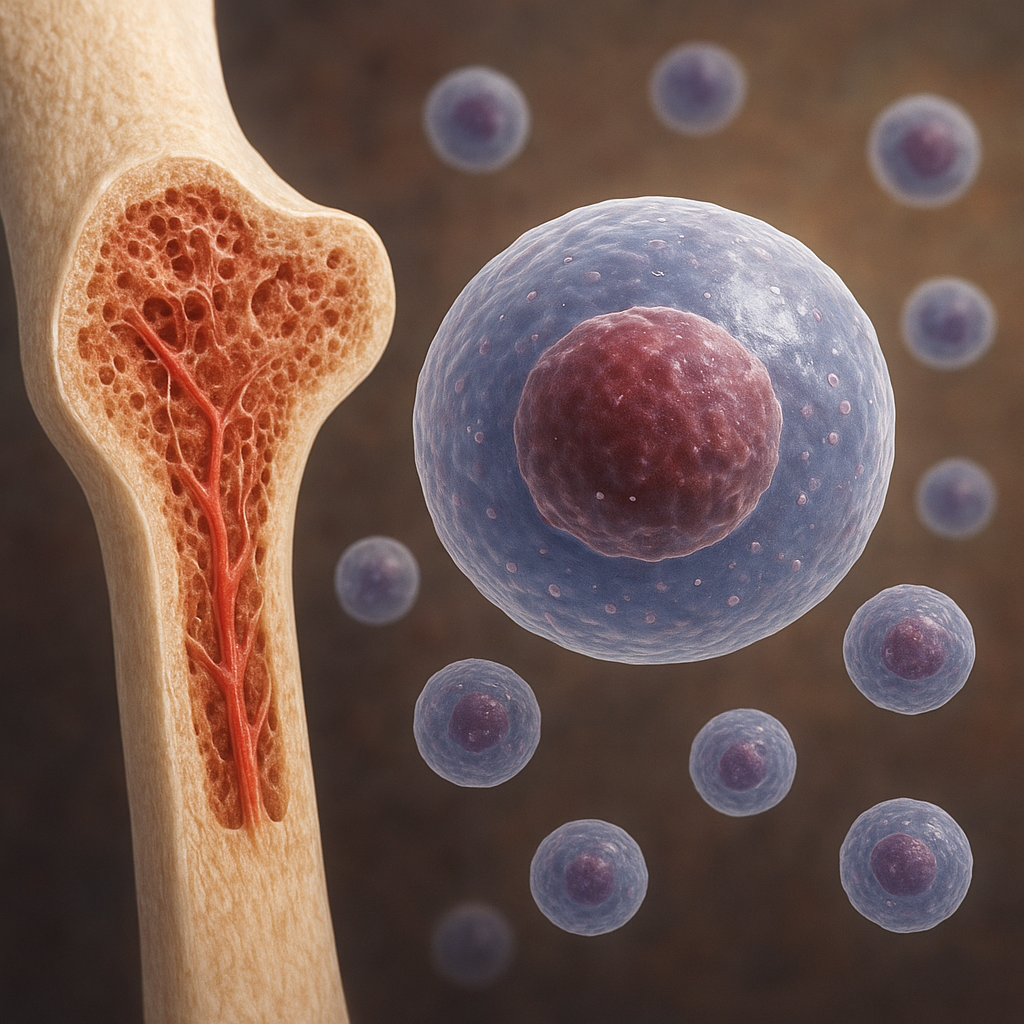
The skeleton is far more than a structural scaffold; it functions as a dynamic endocrine organ. Osteoblasts and osteoclasts orchestrate continuous remodeling, ensuring maintenance of bone strength and mineral homeostasis. Dysregulation of this process can manifest not only as osteoporosis but also as vascular calcification. Both conditions share common molecular cues and systemic influences.
Endocrine Regulators
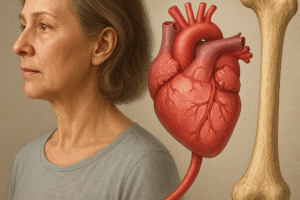
Hormones such as parathyroid hormone (PTH), vitamin D, and estrogen have pivotal roles in skeletal health. PTH modulates calcium resorption from bone, while active vitamin D enhances intestinal absorption of minerals. Deficient vitamin D levels are associated with endothelial dysfunction, a precursor to atherosclerosis. Estrogen deficiency, common in postmenopausal women, accelerates bone loss and may exacerbate lipid abnormalities, raising cardiovascular risk.
Osteoimmunology and Vascular Inflammation
Inflammation is central to both bone resorption and arterial plaque formation. Proinflammatory cytokines, including tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6), stimulate osteoclastogenesis and foster the recruitment of macrophages to arterial walls. Chronic inflammatory states such as rheumatoid arthritis illustrate how systemic immune activation can heighten the incidence of both fractures and myocardial infarction.
Mechanisms Linking Bone Fragility to Vascular Pathology
Several biochemical and cellular mechanisms underpin the association between bone fragility and cardiovascular pathology. Understanding these shared pathways may unveil novel biomarkers and therapeutic targets.
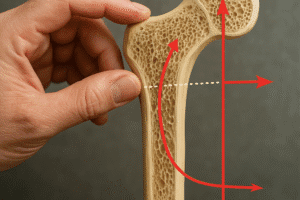
Calcium Paradox: From Bones to Arteries
The “calcium paradox” describes concurrent bone demineralization and vascular calcification. As bone loses mineral density, excess calcium may deposit within the arterial media. Matrix Gla protein (MGP), a vitamin K–dependent inhibitor of calcification, is underexpressed under certain pathological conditions. Insufficient MGP activity contributes to both osteoporosis and arterial stiffening.
Role of Matrix Metalloproteinases
Matrix metalloproteinases (MMPs) degrade extracellular matrix components. In the skeleton, MMPs facilitate normal bone remodeling. However, overexpression of MMP-2 and MMP-9 can accelerate plaque destabilization in atherosclerosis, increasing the risk of acute coronary events. Therapeutic modulation of MMPs is being investigated to preserve bone mass while stabilizing vascular lesions.
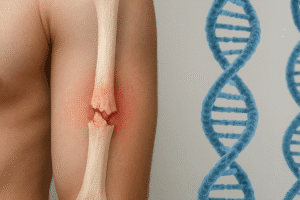
Shared Genetic Factors
- Polymorphisms in the SOST gene (encoding sclerostin) affect bone formation and may influence vascular calcification propensity.
- Variants of the LDLR gene, classically linked to familial hypercholesterolemia, have been associated with alterations in bone mineral density.
- Mutations in the COL1A1 gene, known for causing osteogenesis imperfecta, may also impact connective tissue integrity in the heart and vasculature.
Clinical Implications and Future Directions
Awareness of the bone–heart axis opens the door to holistic approaches in patient care. Screening strategies that combine assessment of bone mineral density with cardiovascular risk profiling could improve early detection of comorbid conditions.
Biomarkers for Dual Risk Assessment
Novel biomarkers under investigation include circulating levels of osteoprotegerin (OPG), fibroblast growth factor-23 (FGF-23), and undercarboxylated osteocalcin. Elevated OPG has been correlated with both fracture risk and coronary artery disease. Meanwhile, high FGF-23, which regulates phosphate metabolism, is linked to arterial stiffness and left ventricular hypertrophy.
Integrated Therapeutic Strategies
- Bisphosphonates—commonly used to inhibit bone resorption—have demonstrated modest vascular benefits in observational studies, potentially by reducing arterial calcification.
- Statins—beyond their lipid‐lowering effects—may exert protective actions on bone through anti‐inflammatory pathways and stimulation of osteoblastic activity.
- Vitamin K supplementation shows promise in reducing undercarboxylated MGP and promoting healthy bone mineralization, while potentially slowing progression of vascular calcification.
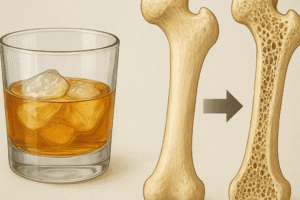
Lifestyle Modification and Prevention
Nonpharmacological interventions remain fundamental. Regular weight-bearing exercise enhances bone density and improves endothelial function. A diet rich in calcium, vitamin D, and antioxidants supports both skeletal and cardiovascular systems. Tobacco cessation and moderation of alcohol intake reduce inflammatory burden and stabilize collagen architecture in bone and vessels.
Emerging Research Frontiers
Advanced imaging modalities, such as high-resolution peripheral quantitative computed tomography (HR-pQCT), can quantify microarchitectural changes in bone and detect early vascular calcifications. Artificial intelligence algorithms applied to large databases may identify novel patterns linking skeletal data to cardiac outcomes, guiding personalized medicine approaches.
In conclusion, the bidirectional influences between bone health and cardiovascular integrity highlight the necessity for interdisciplinary collaboration. As research elucidates the molecular crosstalk and clinical overlaps, healthcare providers will be better equipped to implement comprehensive screening and combined therapies, ultimately improving patient outcomes in both domains.