Long-term immobilization poses a unique threat to the human **skeletal** system, leading to rapid declines in **bone health** and substantial increases in fracture risk. Patients confined to bed rest, orthopedic casts, or space environments often exhibit accelerated bone resorption that outpaces formation. This article explores the underlying mechanisms, identifies key **risk factors**, and presents evidence-based strategies aimed at **preventing** and mitigating bone loss during extended periods of immobility.
Understanding Bone Loss in Immobilization
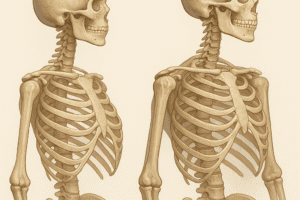
Pathophysiology of Disuse Osteoporosis
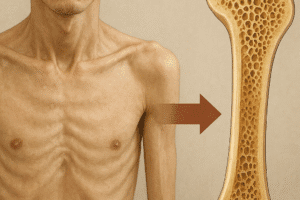
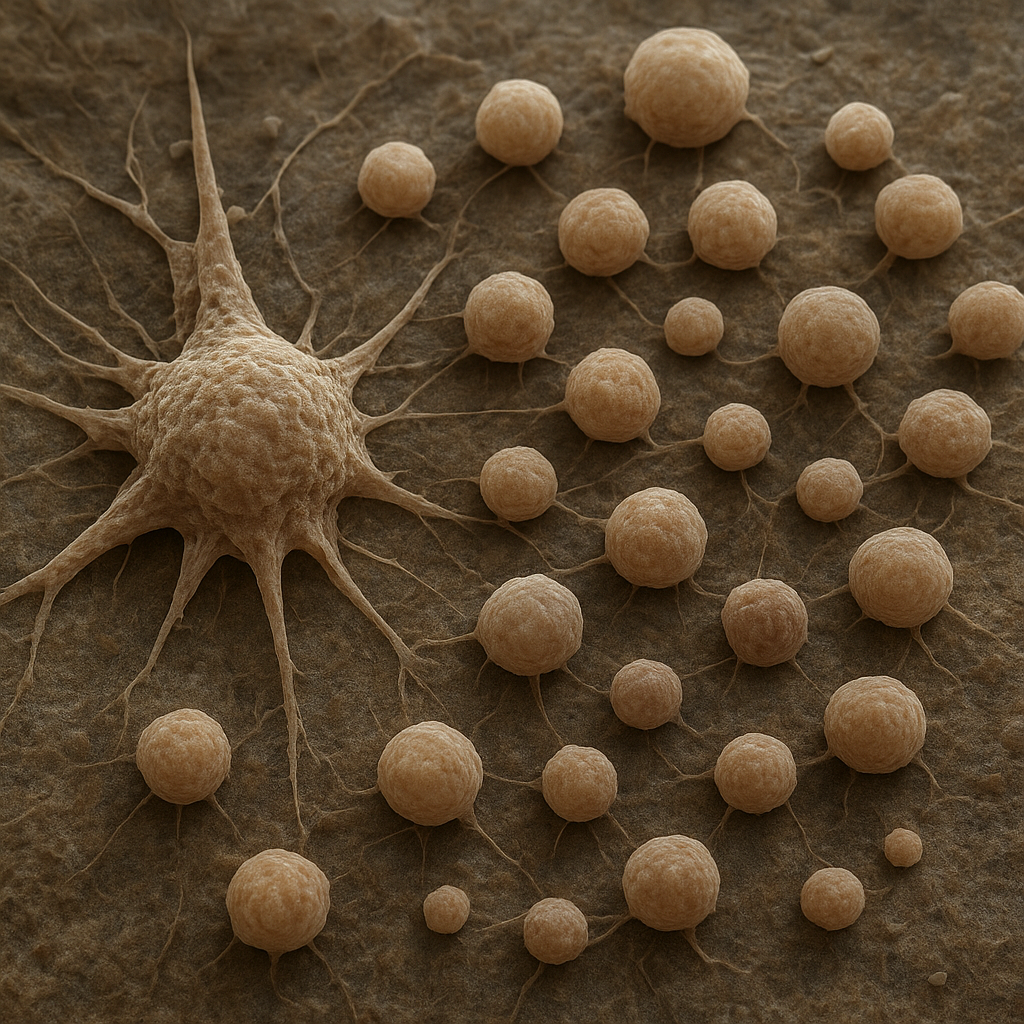
When mechanical forces are removed, skeletal remodeling shifts toward net catabolism. Osteoblast activity declines while **osteoclast activity** increases, resulting in reduced bone mineral density (BMD). This phenomenon, termed disuse osteoporosis, can manifest within weeks of immobilization. The following factors contribute to this imbalance:
- Downregulation of **mechanotransduction** pathways in osteocytes
- Altered expression of RANKL (Receptor Activator of Nuclear Factor κB Ligand) and osteoprotegerin
- Increased inflammatory cytokines (e.g., IL-6, TNF-α) that promote resorption
Clinical Manifestations and Diagnostics
Patients often remain asymptomatic until significant bone loss has occurred. Diagnostic tools include dual-energy X-ray absorptiometry (DEXA) and quantitative computed tomography (QCT), which can detect early declines in volumetric and areal BMD. Biomarkers such as serum C-terminal telopeptide (CTX) and procollagen type 1 N-terminal propeptide (P1NP) may provide dynamic insight into bone turnover rates.
Prevention Strategies
Mechanical Stimulation Techniques
Mechanical loading is the primary stimulus for bone formation. In immobilized patients, alternative methods can substitute for normal weight-bearing:
- Neuromuscular electrical stimulation (NMES) to evoke muscle contractions and generate tensile forces on bone
- Low-intensity vibration therapy that applies oscillatory mechanical signals to the skeleton
- Passive range-of-motion exercises supervised by physical therapists
These interventions aim to activate **mechanical loading** pathways and preserve trabecular architecture.
Nutritional and Lifestyle Interventions
Optimizing **nutritional intake** is essential to support bone matrix production. Core dietary recommendations include:
- Calcium (1,000–1,200 mg/day) through dietary sources or supplementation
- Vitamin D (800–1,000 IU/day) to enhance intestinal calcium absorption and modulate immune-mediated bone turnover
- Protein intake of 1.0–1.2 g/kg body weight to sustain collagen synthesis
- Micronutrients such as magnesium, vitamin K2, and zinc for enzymatic co-factors in bone mineralization
Additionally, avoidance of **smoking** and excessive alcohol can help reduce secondary contributors to bone loss.
Pharmacological Agents
When conservative measures are insufficient, targeted drug therapies may be warranted. Commonly used agents include:
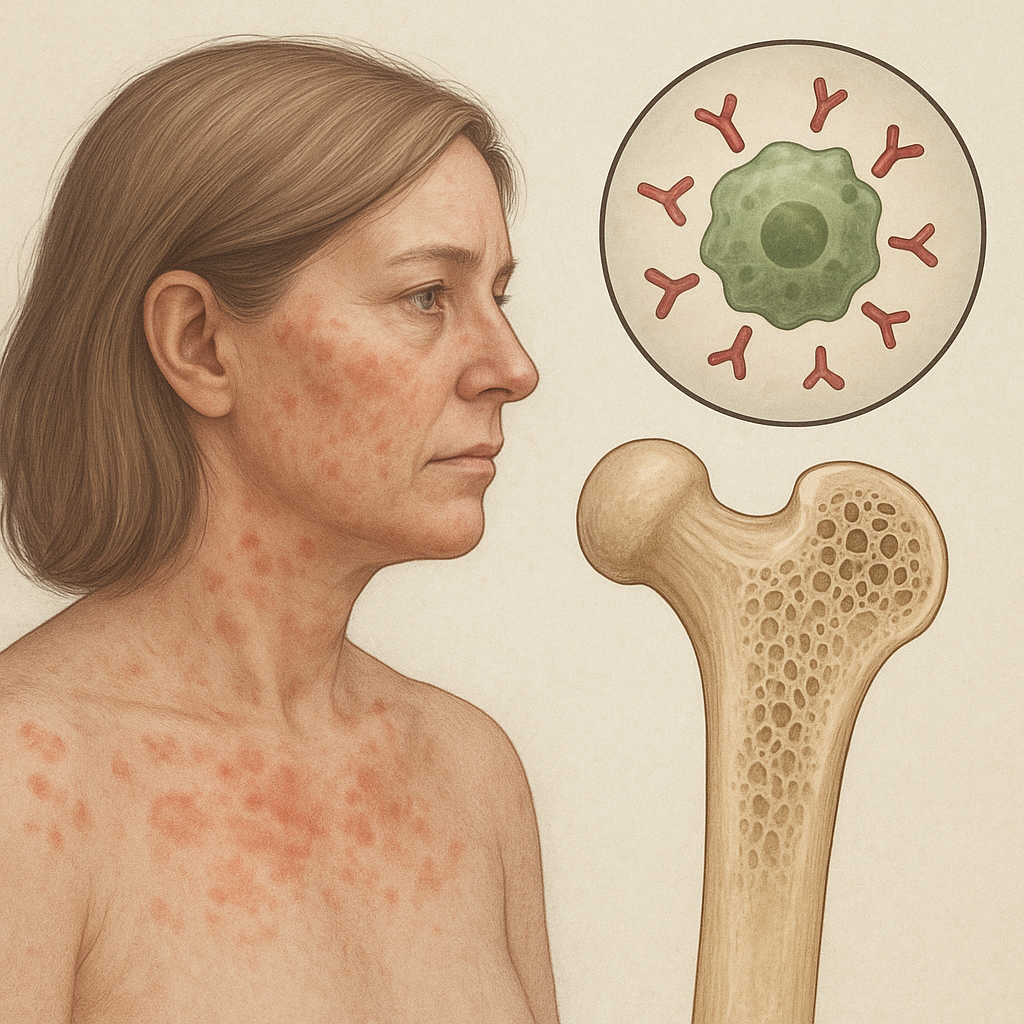
- Bisphosphonates (e.g., alendronate, risedronate) that inhibit osteoclast-mediated bone resorption
- Denosumab, a monoclonal antibody against RANKL, to reduce osteoclast formation
- Teriparatide, a recombinant PTH analog, which transiently stimulates bone formation
- Selective estrogen receptor modulators (SERMs) in postmenopausal women to mimic estrogen’s protective effects
Choice of **pharmacological agents** depends on patient age, sex, comorbidities, and fracture history. Monitoring for side effects—such as osteonecrosis of the jaw with bisphosphonates—is critical to ensure safety.
Clinical Implementation and Challenges
Protocol Development
Effective protocols integrate **physical therapy** with dietary and pharmacological regimens. Multidisciplinary teams should establish individualized plans that specify:
- Frequency and intensity of mechanical loading sessions
- Nutrition counseling and supplementation schedules
- Monitoring timelines for BMD assessments and biochemical markers
Barriers to Adherence
Patient adherence is often compromised by pain, cognitive impairment, or lack of resources. Strategies to improve compliance include:
- Engaging family members and caregivers in education
- Utilizing telemedicine platforms for remote supervision
- Implementing motivational interviewing to address ambivalence
Future Directions in Research and Innovation
Emerging technologies offer promise for more effective preservation of skeletal integrity during periods of immobility. Investigational areas encompass:
- Biomimetic scaffolds that deliver osteoinductive factors directly to bone surfaces
- Gene therapies targeting Wnt/β-catenin signaling to upregulate osteoblast differentiation
- Wearable exoskeletons that facilitate partial weight-bearing movements
- Advanced imaging modalities capable of detecting microarchitectural deterioration before frank BMD loss
Collaborative efforts between basic scientists, clinicians, and biomedical engineers will be crucial to translate these innovations into clinical practice and reduce the burden of osteoporosis associated with **immobilization**.