Maintaining bone density and resilience is a pivotal aspect of overall health, especially as we age. A well-rounded approach to nutrition can significantly mitigate the risk of osteoporosis and fractures. This article delves into evidence-based dietary strategies and lifestyle adjustments designed to fortify your skeletal system, offering practical guidance for achieving lifelong bone strength.
Essential Nutrients for Bone Health
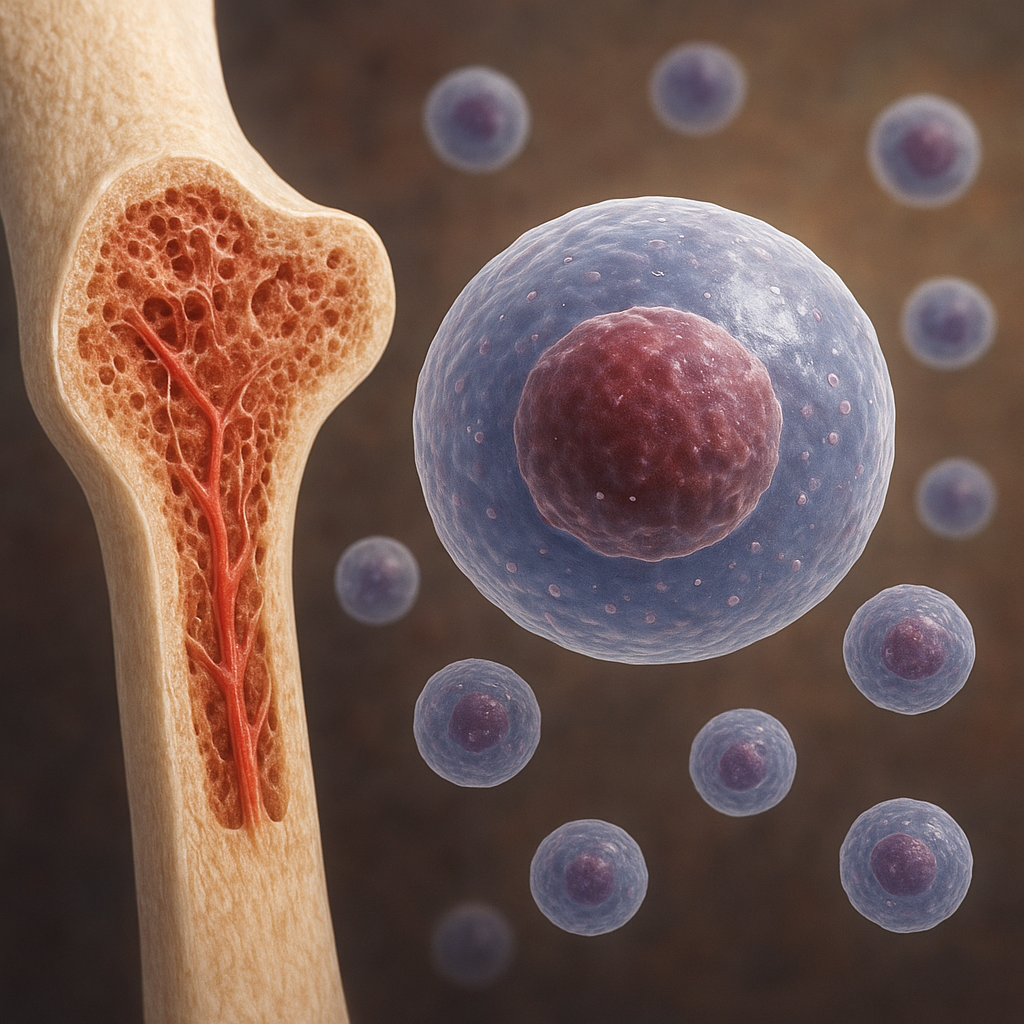
Building and preserving a robust skeletal framework depends on a combination of macronutrients and micronutrients. While calcium often steals the spotlight, other elements such as vitamin D, magnesium, and trace minerals play indispensable roles. Understanding how these nutrients work together is the cornerstone of an effective bone-supportive diet.
Calcium and Its Bioavailability
- Calcium serves as the primary mineral in the bone matrix, providing rigidity and structure.
- Recommended daily intake ranges from 1,000 to 1,300 mg for most adults, depending on age and sex.
- Strategies to enhance absorption:
- Pair calcium-rich foods with vitamin D sources.
- Limit intake of high-oxalate foods (e.g., spinach) at the same meal to avoid interference.
- Avoid excessive caffeine and sodium, which can increase urinary calcium excretion.
Vitamin D: The Sunshine Vitamin
- Acts as a hormone to regulate calcium and phosphorus levels in blood.
- Optimal serum levels are generally between 30–50 ng/mL, ensuring adequate absorption from the gut.
- Primary sources:
- Endogenous synthesis via skin exposure to sunlight.
- Dietary items like fatty fish (salmon, mackerel), egg yolks, and fortified dairy products.
- Supplements: often recommended in northern latitudes or for individuals with limited sun exposure.
Magnesium and Phosphorus Balance
Magnesium aids in the conversion of vitamin D into its active form and assists in parathyroid hormone regulation. Phosphorus works in tandem with calcium to form hydroxyapatite crystals, but excessive phosphorus—common in processed foods—can disrupt the calcium-to-phosphorus ratio, undermining bone density.
Dietary Sources and Meal Planning
A strategic meal plan ensures that essential nutrients are delivered consistently throughout the day. Incorporating a variety of whole foods maximizes the potential for absorption and utilization.
Top Calcium-Rich Foods
- Dairy: yogurt, cheese, milk (preferably low-fat options).
- Fortified plant milks: almond, soy, or oat beverages with added minerals.
- Leafy greens: kale, bok choy, and broccoli (lower in oxalates than spinach).
- Seeds and nuts: chia seeds, almonds, and sesame seeds.
Vitamin D-Boosting Meals
- Grilled salmon with a squeeze of lemon to enhance flavor and zinc absorption.
- Omelet featuring egg yolks, mushrooms, and spinach.
- Bowl of fortified cereal topped with berries and a serving of fortified plant milk.
Integrating Protein Without Compromising Bone Health
Adequate protein intake supports collagen formation in the bone matrix. Aim for 0.8–1.0 g of protein per kg of body weight, prioritizing lean sources that also provide bone-friendly nutrients:
- Poultry and lean red meat
- Fish, especially those high in omega-3 fatty acids
- Legumes and tofu, both rich in magnesium and plant-based protein
Lifestyle and Physical Activity for Bone Strength
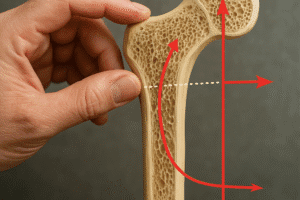
Nutrition and exercise go hand in hand. Weight-bearing activities stimulate bone remodeling, while certain lifestyle habits can either bolster or impair skeletal health.
Weight-Bearing and Resistance Training
- High-impact exercises: jumping rope, plyometrics, and dancing develop bone density in the legs and spine.
- Resistance training: weightlifting and bodyweight exercises help maintain structural integrity and prevent bone loss.
- Frequency: aim for at least three sessions per week, allowing for recovery.
Role of Balance and Flexibility
Practices such as yoga and tai chi enhance proprioception and muscle coordination, reducing fall risk—a key factor in fracture prevention among older adults.
Avoiding Detrimental Habits
- Tobacco smoking accelerates bone resorption and impairs blood flow to bone tissue.
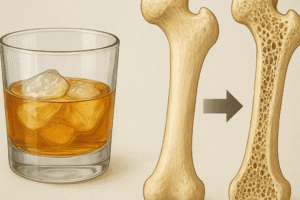
- Excessive alcohol intake disrupts calcium absorption and hormone levels.
- Chronic stress elevates cortisol, which can lead to bone density loss over time.
Targeted Strategies for Special Populations
Certain groups have unique needs and vulnerabilities when it comes to bone health. Tailoring nutritional approaches can optimize outcomes in:
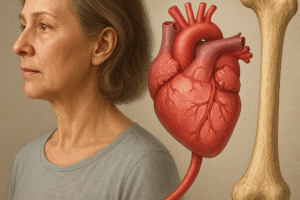
Postmenopausal Women
Estrogen decline dramatically affects bone turnover. Incorporating soy isoflavones, phytoestrogens, and maintaining sufficient vitamin D levels can help moderate bone loss during this transition.
Elderly Individuals
Aging reduces the efficiency of nutrient absorption and vitamin D synthesis. Strategies include:
- Smaller, frequent meals fortified with essential minerals.
- Vitamin D supplementation under clinical supervision.
- Assistance with weight-bearing activities, possibly under the guidance of a physiotherapist to ensure safety.
Adolescents and Young Adults
Achieving peak bone mass before age 30 is critical. Emphasis should be on balanced diets rich in dairy, lean proteins, fruits, and vegetables, combined with regular physical activity to lay the foundation for future bone health.