The integration of nanotechnology into bone regeneration represents a transformative approach in tissue engineering and biomaterials science. By harnessing the unique properties of materials at the nanoscale, researchers are creating advanced platforms that promote rapid osteogenesis, enhance biocompatibility, and enable precise delivery of growth factors. This article explores key aspects of nano‐enabled bone repair, from scaffold design and cellular interplay to clinical translation and safety.
Nanomaterials and Scaffold Design
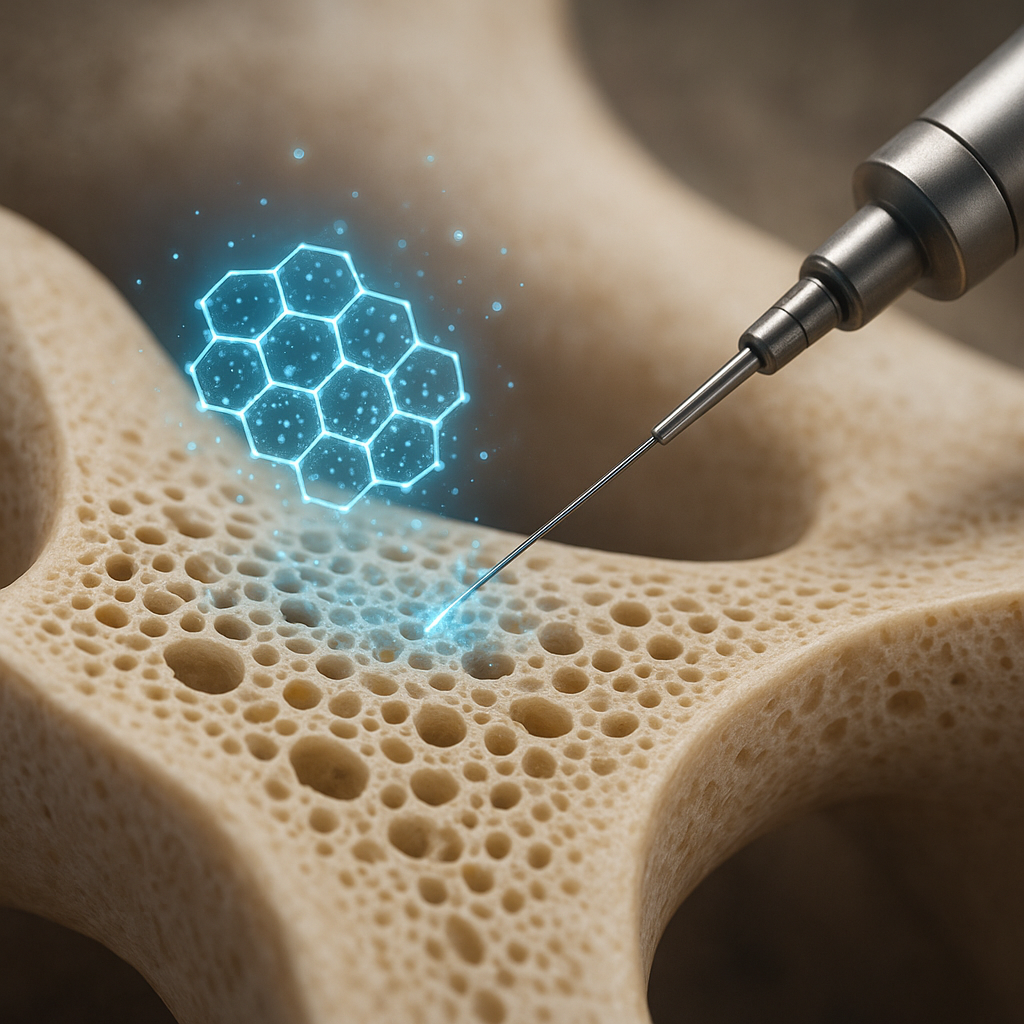
Scaffold architecture lies at the heart of bone tissue engineering. Nanoscale features can mimic the natural extracellular matrix, guiding cell adhesion, proliferation, and differentiation. Recent advances include:
- Nanoparticles incorporated into polymer matrices, creating composite scaffolds that combine mechanical strength with bioactivity.
- Electrospun nanofibers that exhibit high surface area, promoting protein adsorption and cell–matrix interactions.
- 3D‐printed frameworks with nanoscale surface roughness, stimulating osteoblast activity and mineral deposition.
Materials Selection
Common nanoscale components include hydroxyapatite, silica, and bioactive glass. Each offers distinct advantages:
- Hydroxyapatite nanoparticles mimic the mineral phase of bone, boosting bioactivity and mechanical stiffness.
- Silica‐based nanoparticles enhance scaffold porosity and support controlled release of therapeutic ions.
- Bioactive glass fosters angiogenesis and vascularization, critical for nutrient supply in regenerating bone.
Functionalization Strategies
Surface modification of nanoscale scaffolds enables targeted interactions:
- Peptide or protein coatings that present cell‐adhesion motifs (e.g., RGD sequences) to promote osteoblast attachment.
- Covalent grafting of growth factors for sustained, localized delivery, minimizing systemic side effects.
- Stimuli‐responsive nanogels that release therapeutic agents under pH or temperature triggers, tailoring treatment to local microenvironments.
Cellular Interactions and Mechanisms
The success of nano‐facilitated bone repair hinges on complex biological processes. At the cellular level, nanoscale topography and chemistry orchestrate key signaling pathways:
Stem Cell Differentiation
Mesenchymal stem cells (MSCs) cultivated on nanostructured surfaces exhibit enhanced lineage commitment toward osteoblasts. Mechanotransduction mechanisms sense nanoscale stiffness and transmit cues through focal adhesion complexes to the nucleus, upregulating osteogenic genes.
Immune Modulation
Macrophages encounter implanted materials first and adopt phenotypes that can either support inflammation or facilitate healing. Nanoscale surface patterns and chemical functionalization can skew macrophage polarization toward an M2 reparative phenotype, reducing fibrotic encapsulation and fostering bone formation.
Angiogenic Support
Bone regeneration demands a robust vascular network. Nanoparticles releasing angiogenic factors like VEGF enhance blood vessel ingrowth, ensuring oxygen and nutrient supply. Co‐delivery of osteoinductive and angiogenic cues in a single nanocomposite scaffold optimizes the healing microenvironment.
Clinical Applications and Future Prospects
Translating nano‐enabled bone therapies into clinical practice requires rigorous evaluation of performance and safety. Several exciting directions include:
- Injectable nanocomposite hydrogels for minimally invasive repair of critical‐size defects in long bones.
- Nanotube‐coated implants that accelerate osseointegration in dental and orthopedic applications.
- Personalized 3D‐printed scaffolds embedded with patient‐derived cells and nanoparticles tailored to specific defect geometries.
Regulatory Pathways
Regulatory agencies demand comprehensive characterization of nanomaterial composition, degradation profiles, and in vivo biodistribution. Standardized protocols for preclinical testing are under development to assess toxicology and long‐term safety.
Emerging Technologies
Future innovations may include:
- Smart scaffolds embedded with nanosensors to monitor pH, oxygen levels, and mechanical load in real time.
- Gene‐activated nanoparticles that deliver osteogenic DNA sequences directly to resident progenitor cells.
- Artificial intelligence–guided design of nanocomposite formulations optimized for individual patient biology.
Challenges and Safety Considerations
Despite promising results, several hurdles remain before widespread adoption:
- Understanding long‐term fate of nanoparticles after scaffold degradation and their interactions with systemic organs.
- Ensuring reproducibility and scalability of nanomaterial synthesis under Good Manufacturing Practice (GMP) conditions.
- Balancing nanoenhancement of mechanical properties with potential cytotoxicity at high particle concentrations.
Continuous collaboration among materials scientists, biologists, clinicians, and regulatory bodies will be essential to navigate these challenges and fully realize the potential of nanotechnology in bone regeneration.