Effective management of pain following bone fracture surgery is essential for a successful recovery, reducing the risk of chronic discomfort, and restoring function. Patients and healthcare providers must collaborate to tailor a comprehensive pain control plan that addresses both immediate postoperative needs and long-term rehabilitation goals. This article explores key strategies to alleviate pain, minimize complications, and foster optimal healing after fracture repair.
Understanding Postoperative Pain Mechanisms
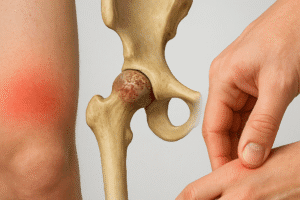
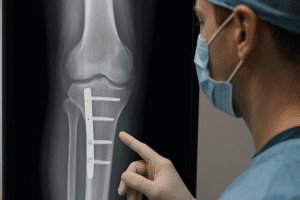
Following fracture surgery, patients experience pain resulting from a combination of factors: soft tissue trauma, bone manipulation, and inflammatory responses. When a fracture is stabilized with plates, screws, or rods, the surrounding nerves and muscles can become irritated. This leads to the release of inflammatory mediators such as prostaglandins and cytokines, which sensitize nerve endings and produce acute pain.
The Inflammatory Cascade
- Initial Tissue Injury: Surgical incisions and bone realignment trigger an immediate release of histamine and bradykinin.
- Immune Activation: Neutrophils and macrophages migrate to the site, secreting pro-inflammatory cytokines (e.g., interleukins, TNF-α).
- Sensitization: Local nerve fibers become hyperexcitable, heightening pain perception and contributing to postoperative hyperalgesia.
Nociceptive and Neuropathic Components
While nociceptive pain arises from tissue damage and inflammation, neuropathic pain may develop if nerves are compressed or entrapped by callus formation or hardware. Recognizing the dual nature of postoperative discomfort is critical for selecting appropriate analgesic regimens.
- Nociceptive pain: Throbbing, aching sensation localized to the surgical site.
- Neuropathic pain: Burning, shooting, or electric shock–like sensations, often indicating nerve involvement.
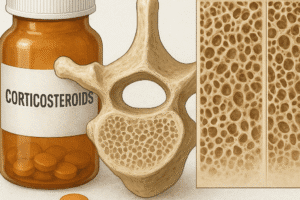
Pharmacological Strategies for Pain Control
Optimal pharmacotherapy combines medications that target different pathways of the pain mechanism. A multimodal approach reduces reliance on any single agent and enhances overall efficacy.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
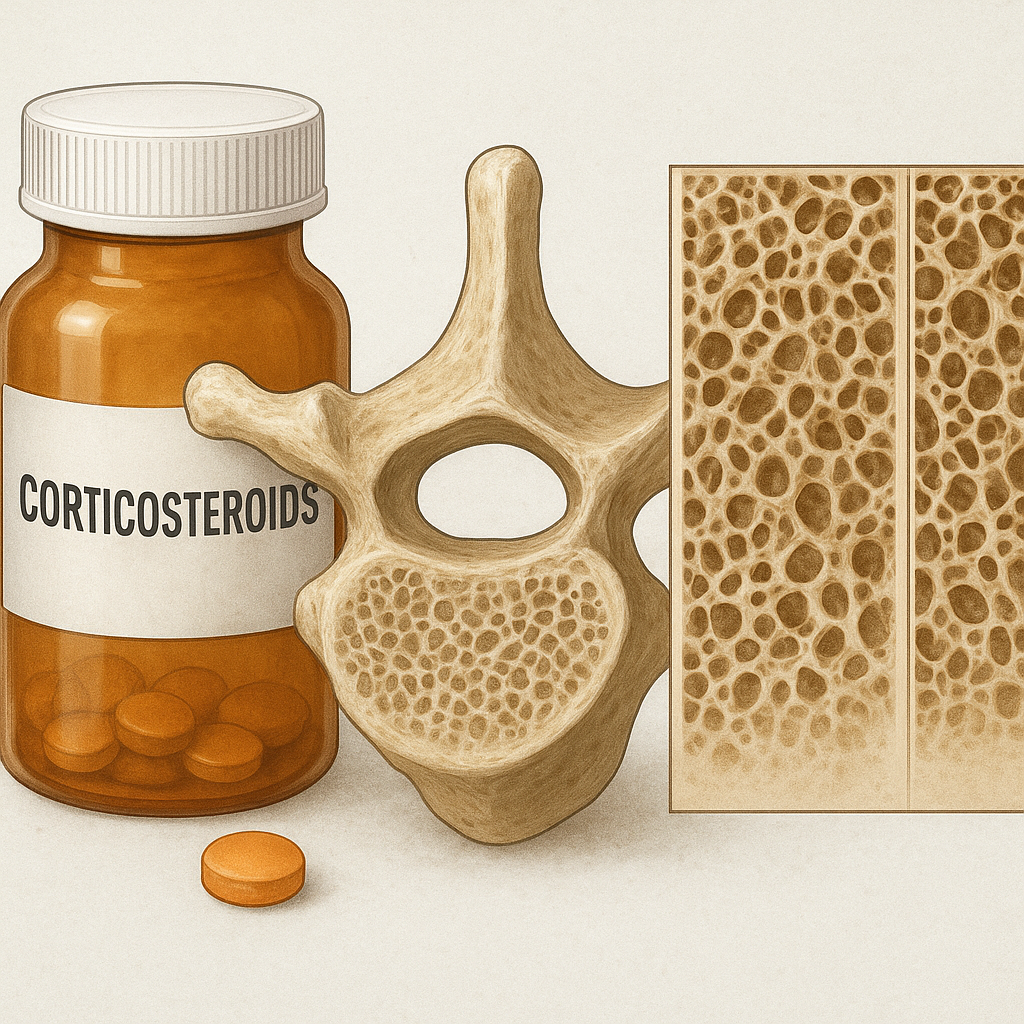
NSAIDs such as ibuprofen, naproxen, and celecoxib inhibit cyclooxygenase enzymes, reducing prostaglandin synthesis and inflammation. They are first-line agents for mild to moderate pain, but clinicians should monitor for gastrointestinal irritation and renal effects.
Opioid Analgesics
For moderate to severe pain, short-term use of opioids (e.g., morphine, oxycodone) may be necessary. Prescribers must balance effective analgesia with the risk of dependency. Implementing taper schedules and combining opioids with non-opioid medications can minimize total dosage.
Adjuvant Medications
- Anticonvulsants (gabapentin, pregabalin): Effective for neuropathic pain by modulating calcium channels in nerve fibers.
- Antidepressants (amitriptyline, duloxetine): Block reuptake of serotonin and norepinephrine, boosting endogenous pain inhibition.
- Local anesthetics (lidocaine patches, bupivacaine wound infiltration): Provide targeted relief with minimal systemic effects.
Non-Pharmacological and Adjunctive Approaches
Complementary therapies can enhance pain relief, reduce medication requirements, and improve patient satisfaction. Combining these methods with pharmacotherapy promotes a holistic recovery.
Physical Therapy and Rehabilitation
Early mobilization under the guidance of a qualified physical therapist prevents joint stiffness, reduces muscle atrophy, and supports circulation. Techniques include:
- Range-of-motion exercises to maintain flexibility and prevent contractures.
- Isometric strengthening to support the affected bone without excessive stress.
- Gait training with assistive devices (crutches, walkers) to ensure safe weight-bearing progression.
Cold and Heat Therapy
Applying ice packs in the first 48–72 hours post-surgery can diminish swelling and numb peripheral nerves. Later, mild heat improves blood flow and relaxes tense muscles surrounding the fracture site.
Transcutaneous Electrical Nerve Stimulation (TENS)
TENS units deliver low-voltage electrical currents to stimulate large-diameter Aβ fibers, which inhibit pain signals transmitted by smaller C fibers. Patients often report decreased pain intensity and reduced need for opioids when TENS is integrated into their regimen.
Mind-Body Techniques
- Guided imagery: Visualization exercises that divert attention away from discomfort.
- Deep breathing and progressive muscle relaxation: Lower stress hormones and muscle tension.
- Biofeedback: Provides real-time data on physiological parameters, enabling patients to regulate their pain response.
Optimizing Rehabilitation and Recovery
Beyond immediate pain control, successful fracture healing requires a multidisciplinary approach emphasizing nutrition, lifestyle modifications, and patient education.
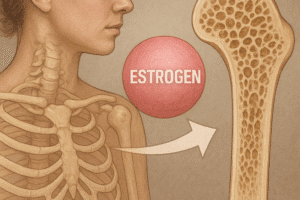
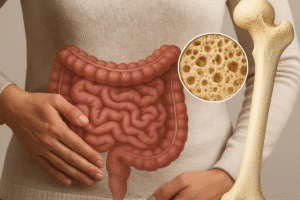
Nutritional Support
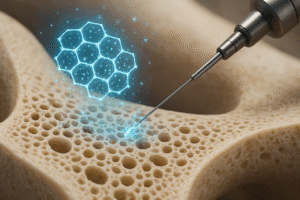
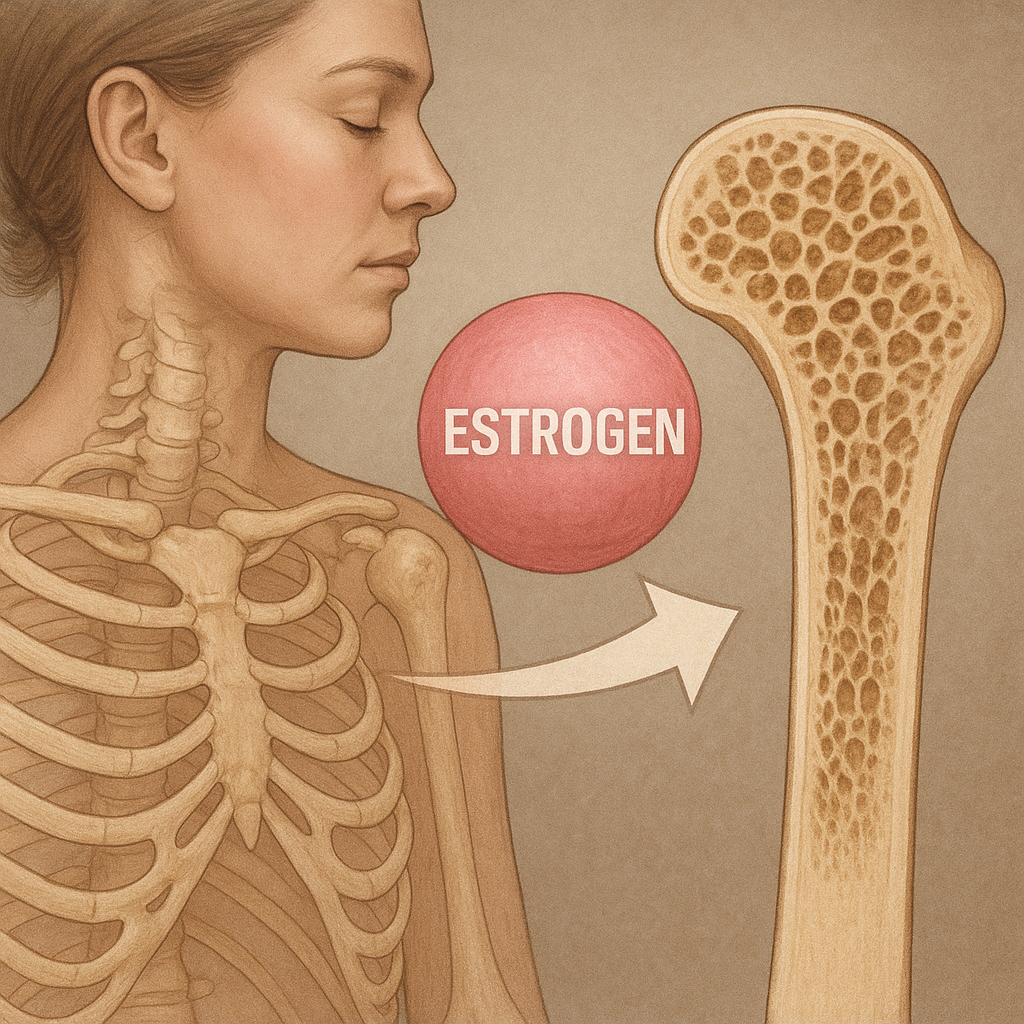
A balanced diet rich in calcium, vitamin D, protein, and micronutrients supports bone remodeling. Supplementation should be considered for patients with deficiencies, especially older adults at risk for osteoporosis.
Monitoring and Managing Complications
- Infection: Vigilant wound care and early antibiotic therapy when indicated.
- Hardware irritation: Periodic imaging to confirm stable fixation and rule out loosening.
- Chronic pain syndromes: Referral to pain specialists for advanced interventions such as nerve blocks or spinal cord stimulation.
Patient Education and Engagement
Empowering patients through information fosters adherence to therapy plans. Topics to address include:
- Recognizing signs of complications (fever, increased swelling, unusual discharge).
- Safe use of analgesics, including potential side effects and avoidance of over-the-counter NSAID overuse.
- The importance of incremental activity progression to prevent deconditioning and promote bone strength.
The Role of a Multidisciplinary Team
Coordinated care involving orthopedic surgeons, anesthesiologists, physiotherapists, dietitians, and pain management specialists ensures that each aspect of the patient’s recovery is addressed. Regular team meetings and clear communication channels optimize outcomes.
By integrating evidence-based pharmacological therapies, complementary modalities, and a structured rehabilitation plan, healthcare providers can significantly reduce postoperative pain, enhance functional recovery, and improve overall quality of life following bone fracture surgery.