Sleep is a vital physiological process that extends far beyond simple rest. In the context of bone health, it acts as a powerful modulator of cellular activity, hormonal release, and overall tissue regeneration. Recent research highlights how insufficient or disrupted sleep impairs critical phases of bone repair, while optimized sleep patterns can accelerate recovery. This article examines the multifaceted relationship between sleep and bone regeneration, emphasizing molecular pathways, hormonal influences, and clinical considerations.
Understanding Bone Remodeling and Sleep
Bone Remodeling Basics
Bone remodeling is an ongoing biological process where old bone is replaced by new bone tissue. Two primary cell types orchestrate this dynamic: osteoclasts (resorption) and osteoblasts (formation). Under normal conditions, these cells maintain skeletal integrity and respond to microdamage or fractures by initiating repair. Sleep significantly influences both phases by modulating cellular proliferation, differentiation, and apoptosis.
Cellular and Molecular Mechanisms
- Osteoblast Activity: During deep sleep phases, especially slow-wave sleep, the proliferation of osteoblast precursors increases. Growth factors like bone morphogenetic proteins (BMPs) are secreted more abundantly, promoting matrix deposition.
- Osteoclast Regulation: Proper sleep reduces sympathetic tone and cortisol levels, both of which otherwise enhance osteoclast-mediated resorption. By downregulating RANKL (receptor activator of nuclear factor kappa-Β ligand), sleep protects against excessive bone breakdown.
- Extracellular Matrix Synthesis: Collagen cross-linking and mineralization depend on circadian-controlled genes. Disruption of the circadian rhythm leads to altered expression of osteocalcin and alkaline phosphatase, compromising matrix quality.
Hormonal Influence Linked to Sleep Quality
Endocrine Modulators of Bone Repair
Sleep governs the release of several hormones that are indispensable for skeletal maintenance. Disruptions in sleep architecture can thus create hormonal imbalances, slowing down the regeneration process.
Growth Hormone and IGF-1
A major surge of growth hormone occurs during slow-wave sleep, stimulating the liver to produce insulin-like growth factor 1 (IGF-1). Both are critical for:
- Enhancing osteoblast proliferation
- Promoting cartilage formation at fracture sites
- Facilitating collagen synthesis and mineral deposition
Melatonin and Bone Density
Melatonin, typically known for regulating sleep–wake cycles, also exerts direct effects on bone. It:
- Inhibits osteoclast genesis
- Reduces oxidative stress in bone marrow
- Improves microarchitecture through antioxidant pathways
Inflammatory Cytokines and Cortisol
Chronic sleep deprivation elevates inflammatory markers such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). These cytokines:
- Enhance osteoclast differentiation
- Delay callus formation
- Impair vascularization at injury sites
At the same time, increased cortisol levels contribute to net bone loss by stimulating RANKL and suppressing osteoblast function.
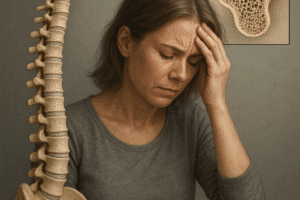
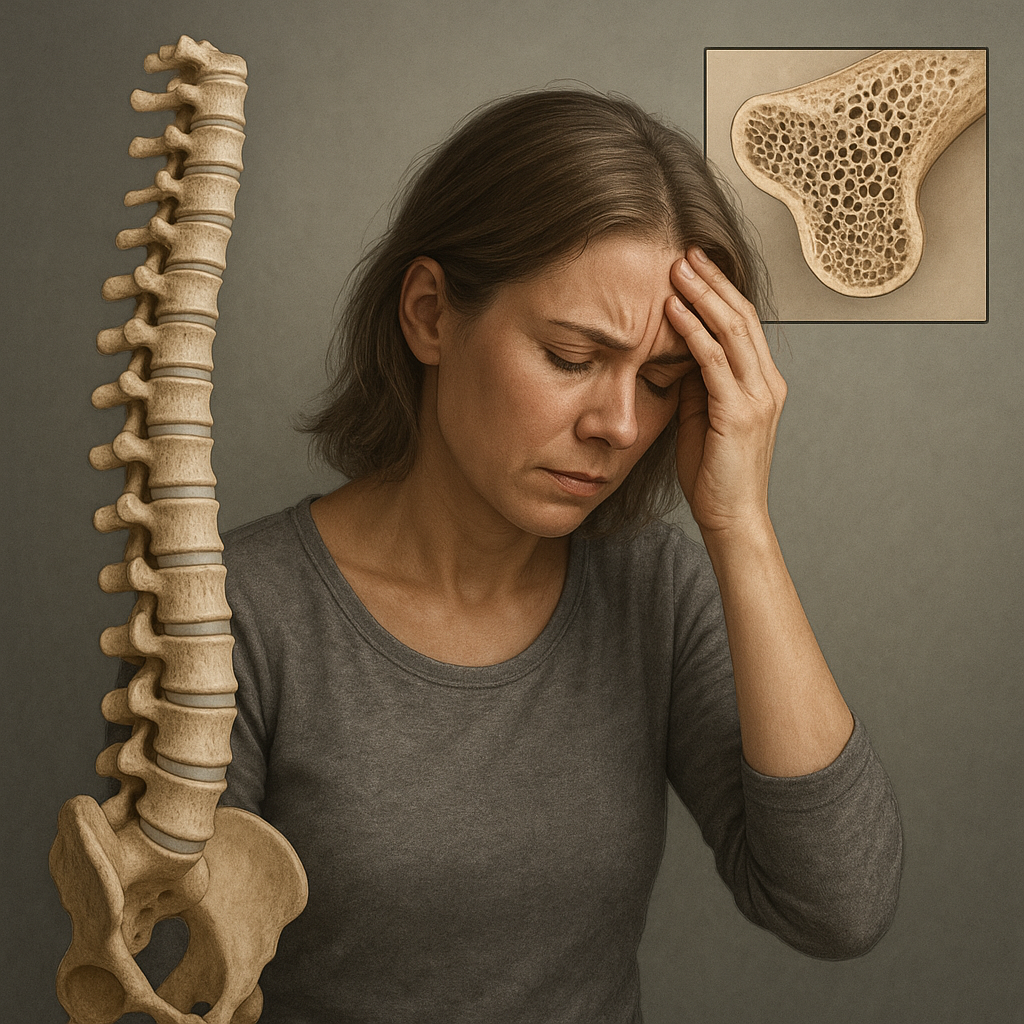
Consequences of Sleep Disorders on Bone Healing
Clinical Evidence from Insomnia and Sleep Apnea
Patients with chronic insomnia or obstructive sleep apnea often present with delayed bone union and reduced bone mineral density (BMD). Multiple cohort studies have reported:
- Up to a 20% longer healing time for fractures in patients reporting less than six hours of sleep per night.
- Lower trabecular thickness and bone volume fraction in individuals with untreated sleep apnea.
- Elevated markers of bone turnover, indicating uncoupled resorption and formation.
Case Study: Postoperative Recovery
In a study of hip replacement patients, those with optimized sleep protocols (pre-surgery sleep hygiene education, postoperative sleep monitoring) experienced:
- Faster restoration of weight-bearing capacity
- Reduced pain scores during the first two weeks
- Higher levels of circulating osteocalcin at one month
Shift Work and Long-Term Skeletal Health
Night-shift workers are at increased risk of osteoporosis later in life. Persistent circadian misalignment disrupts endocrine cycles and lowers peak bone mass by:
- Reducing peak calcium absorption during daytime hours
- Altering parathyroid hormone rhythms
- Increasing chronic low-grade inflammation
Strategies to Optimize Sleep for Bone Regeneration
Sleep Hygiene and Lifestyle Interventions
Given the strong link between restorative sleep and bone health, clinicians should recommend tailored interventions:
- Consistent sleep schedule: Aim for 7–9 hours per night to maximize slow-wave phases.
- Sleep environment: Maintain cool, dark, and quiet surroundings to facilitate uninterrupted cycles.
- Pre-sleep routine: Limit blue-light exposure and avoid stimulants at least two hours before bedtime.
Pharmacological and Nutritional Support
In select cases, short-term use of melatonin supplements may restore normal sleep architecture. Additionally:
- Ensure adequate intake of vitamin D and calcium to support mineralization.
- Consider anti-inflammatory nutrients (omega-3 fatty acids) to mitigate cytokine-driven bone resorption.
- Monitor hormone levels in patients with endocrine disorders to tailor therapy.
Integrating Sleep Monitoring into Orthopedic Care
Emerging wearable technologies allow real-time tracking of sleep stages and duration. Incorporating these data into postoperative protocols can:
- Identify patients at risk for impaired healing due to fragmented sleep.
- Enable early interventions to correct sleep disturbances.
- Correlate sleep metrics with biomarkers of bone turnover for personalized recovery plans.
The Interplay of Immune Function and Sleep in Bone Repair
Immunomodulation During Sleep
Sleep fosters an environment conducive to immunoregulatory processes essential for bone healing. During deep sleep:
- Immune function shifts toward tissue repair, with macrophages clearing debris and secreting pro-regenerative factors.
- T Regulatory cells expand, controlling excessive inflammation that can disrupt callus formation.
- Enhanced lymphatic flow aids in nutrient delivery and waste removal from fracture sites.
Microenvironment Dynamics
The bone marrow niche is highly sensitive to systemic cues. Sustained sleep deprivation:
- Impairs hematopoietic stem cell differentiation
- Alters local oxygen tension, reducing angiogenesis
- Leads to fibrotic tissue deposition instead of healthy bone matrix
Future Directions in Research
Ongoing studies aim to elucidate:
- The role of specific sleep stages in regulating osteoimmunology.
- Genetic markers that predict individual responses to sleep-based interventions.
- Novel therapeutics mimicking sleep-induced growth factor profiles.