Proper nutrition plays a pivotal role in supporting the complex process of bone regeneration following surgical intervention. Surgical repair of fractures or orthopedic procedures sets in motion a cascade of cellular and molecular events aimed at restoring structural integrity. While surgical technique and postoperative care are crucial, the influence of diet on healing cannot be overstated. This article explores how targeted dietary strategies can optimize recovery, enhance bone density, and minimize complications.
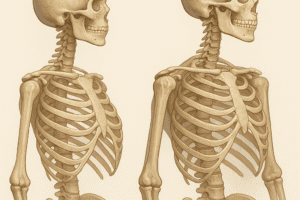
Understanding the Biology of Bone Repair
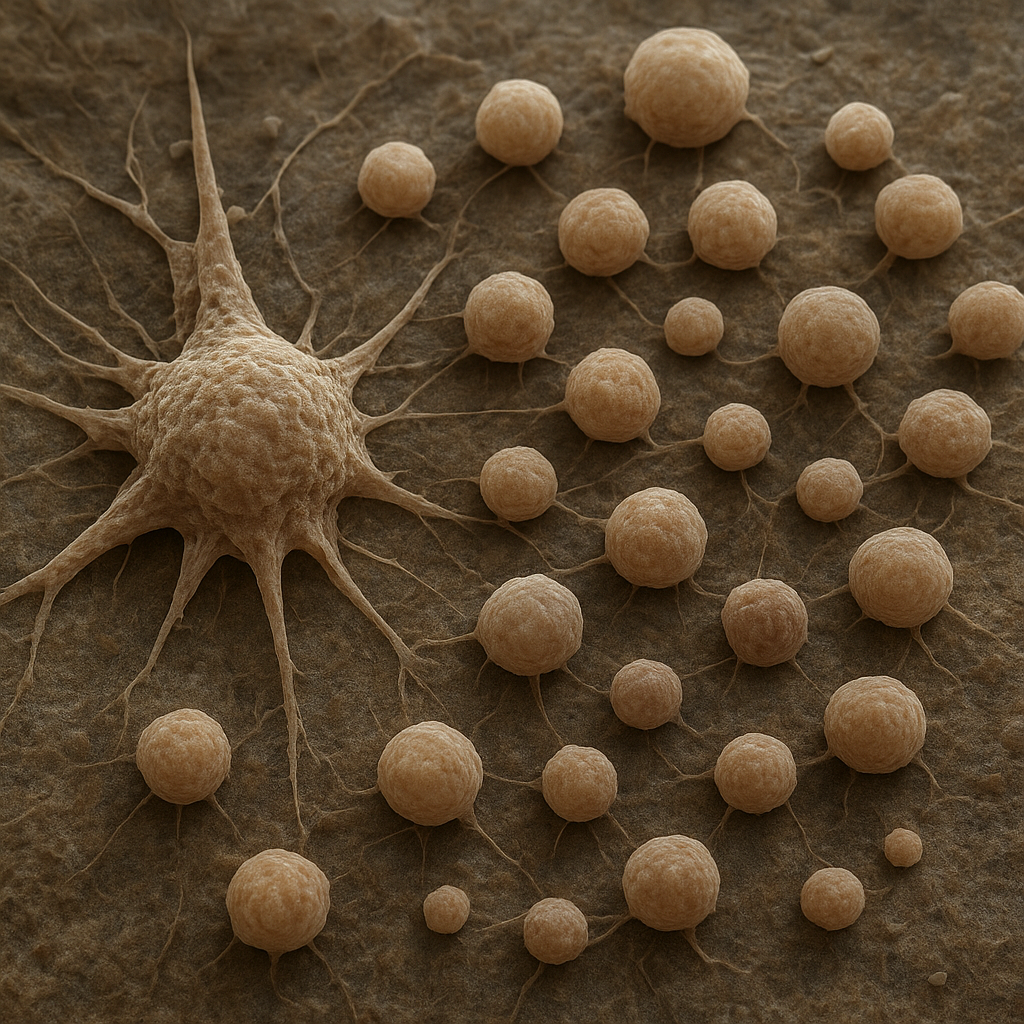
Bone healing after surgery unfolds in three overlapping phases: inflammation, repair, and remodeling. During the initial inflammation phase, immune cells clear debris and secrete cytokines that recruit mesenchymal stem cells. In the subsequent repair stage, these progenitor cells differentiate into osteoblasts, producing a collagen-rich matrix that gradually mineralizes. Finally, during remodeling, woven bone is replaced by lamellar bone, restoring original strength and shape. Throughout these stages, specific nutrients serve as building blocks and signaling factors essential for each step.
Key Nutrients and Their Roles
- Calcium: As the primary mineral in bone, calcium ions combine with phosphate to form hydroxyapatite crystals that harden the matrix. Adequate calcium intake ensures a steady supply for mineralization during the repair phase.
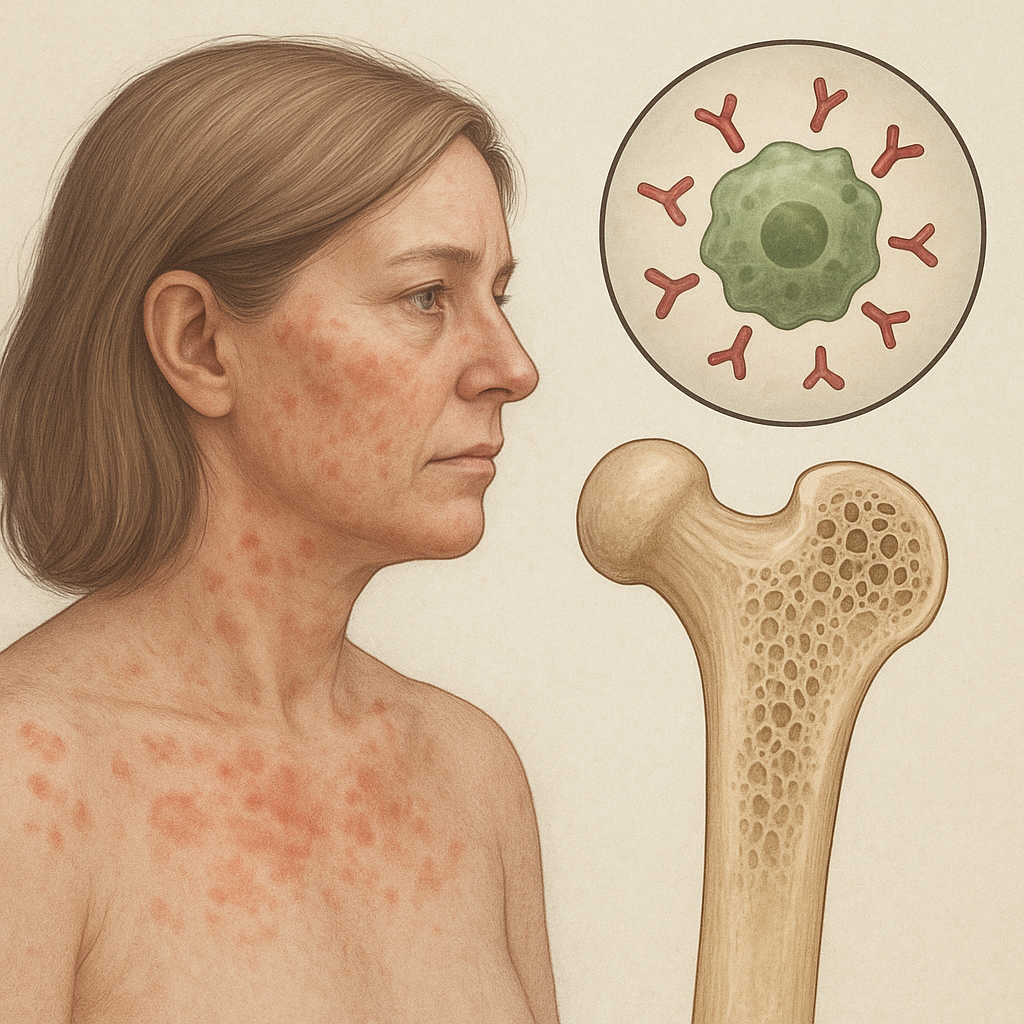
- Vitamin D: This secosteroid hormone enhances intestinal absorption of calcium and phosphate. Active vitamin D metabolites also regulate osteoblast and osteoclast activity, balancing bone formation and resorption.
- Protein: Collagen fibers form the organic scaffolding for new bone. Dietary protein provides essential amino acids—especially glycine, proline, and lysine—for collagen synthesis and repair of soft tissues.
- Collagen Supplements: Hydrolyzed collagen peptides may support matrix formation by directly supplying collagen subunits, potentially accelerating callus development in the repair phase.
- Minerals such as magnesium, zinc, and phosphorus participate in enzymatic reactions that cross-link collagen and crystallize bone mineral. Each element plays a nonredundant role in bone architecture and strength.
- Vitamin C: A cofactor for prolyl and lysyl hydroxylases, vitamin C is indispensable in stabilizing and cross-linking collagen fibrils during bone matrix maturation.
- B Vitamins: Riboflavin and niacin contribute to cellular energy metabolism, supporting the high demands of proliferating osteoblasts.
- Omega-3 Fatty Acids: Found in fish oil, these lipids exhibit anti-inflammatory properties, potentially mitigating excessive inflammation that could delay healing.
- Vitamin K2: This vitamin directs calcium binding to bone rather than soft tissues by activating osteocalcin, a protein secreted by osteoblasts.
- Polyphenols: Plant-derived antioxidants protect osteoprogenitor cells from oxidative stress and support the synthesis of growth factors involved in bone regeneration.
Impact of Macro- and Micronutrients on Healing Phases
Inflammatory Phase
During the first few days post-surgery, a well-modulated inflammatory response is vital. Nutrients with inflammation reduction properties—such as omega-3 fatty acids, vitamin E, and polyphenols—help prevent chronic inflammation that can impair healing. A balanced intake of lean proteins supports immune cell function and provides amino acids for early matrix deposition.
Repair Phase
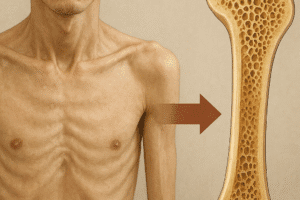
Once the inflammatory cascade subsides, osteoblasts begin to synthesize a new collagen network. Adequate protein and vitamin C are crucial here. Concurrently, sufficient levels of calcium and vitamin D ensure proper mineralization. A deficiency in any of these nutrients can result in a weak callus and delayed union.
Remodeling Phase
Over months, the immature callus is reshaped into mature lamellar bone. This remodeling demands sustained supplies of minerals and vitamins, as well as mechanical loading through physiotherapy. Dietary strategies that preserve bone mass—such as inclusion of vitamin K2 for appropriate calcium utilization—support long-term outcomes and reduce the risk of stress fractures or osteoporosis at the surgical site.
Dietary Patterns and Bone Repair
Beyond individual nutrients, holistic dietary approaches can synergize to optimize healing:
- Traditional Mediterranean Diet: Rich in fruits, vegetables, whole grains, lean proteins, and olive oil, this pattern supplies ample antioxidants, anti-inflammatory lipids, and plant-based polyphenols. Trials indicate improved bone turnover markers and fracture healing rates.
- High-Protein Diets: Customized to deliver 1.2–1.5 g/kg body weight per day in post-surgical patients, ensuring effective collagen synthesis without excessive renal load.
- Fortified Regimens: Incorporating dairy or alternative milk products fortified with calcium and vitamin D can address deficiencies common in elderly or hospitalized individuals.
- Low-Glycemic Index Foods: Stabilizing blood sugar levels prevents glycation of collagen, which can reduce matrix quality and slow healing.
Practical Recommendations for Post-Surgical Patients
To harness the benefits of nutrition in bone regeneration, consider the following guidelines:
- Consult with a registered dietitian or clinician to tailor nutrient intake based on individual risk factors such as age, comorbidities, and baseline bone health.
- Ensure daily intake of at least 1,000–1,200 mg of calcium and 800–2,000 IU of vitamin D, adjusting for serum levels and sun exposure.
- Consume 20–30 g of high-quality protein per meal, focusing on lean meats, dairy, legumes, and plant-based sources.
- Include two to three servings of oily fish weekly for omega-3 fatty acids and anti-inflammatory effects.
- Incorporate colorful fruits and vegetables to supply antioxidants, polyphenols, and fiber that promote a healthy microbiome, which in turn may influence bone metabolism.
- Stay hydrated to support nutrient transport and cellular homeostasis in healing tissues.
- Monitor and manage potential drug–nutrient interactions, especially with corticosteroids or proton-pump inhibitors that can affect mineral absorption.
- Engage in physician-approved weight-bearing and resistance exercises as part of rehabilitation to stimulate bone remodeling and vascularization at the surgical site.
- Consider targeted supplementation—such as collagen peptides or vitamin K2—under professional supervision when dietary intake is insufficient.
Factors That May Impede Nutritional Support
Surgical patients often face hurdles that compromise optimal nutrient status:
- Reduced appetite, nausea, or swallowing difficulties post-anesthesia.
- Malabsorption syndromes or gastrointestinal surgeries that limit absorption of key vitamins and minerals.
- Chronic conditions like diabetes or renal insufficiency that impose dietary restrictions.
- Use of medications that alter bone metabolism or impair nutrient bioavailability.
Addressing these factors through proactive dietary planning and, if necessary, medical nutrition therapy ensures that the fracture repair process proceeds without avoidable delays or complications.
Emerging Research and Future Directions
Novel strategies are under investigation to further enhance post-surgical bone healing. These include:
- Personalized nutrition plans guided by genetic profiling and biomarkers of bone turnover.
- Functional foods enriched with bioactive peptides or phytoestrogens designed to target osteoblastogenesis.
- Probiotic interventions aimed at modulating gut microbiota to influence mineral absorption and systemic inflammation.
- Nanotechnology-based nutrient delivery systems for localized, sustained release of growth factors and minerals at the repair site.
While these approaches remain largely experimental, they underscore the growing recognition that dietary interventions represent a potent, noninvasive complement to surgical and pharmacological therapies in bone medicine.