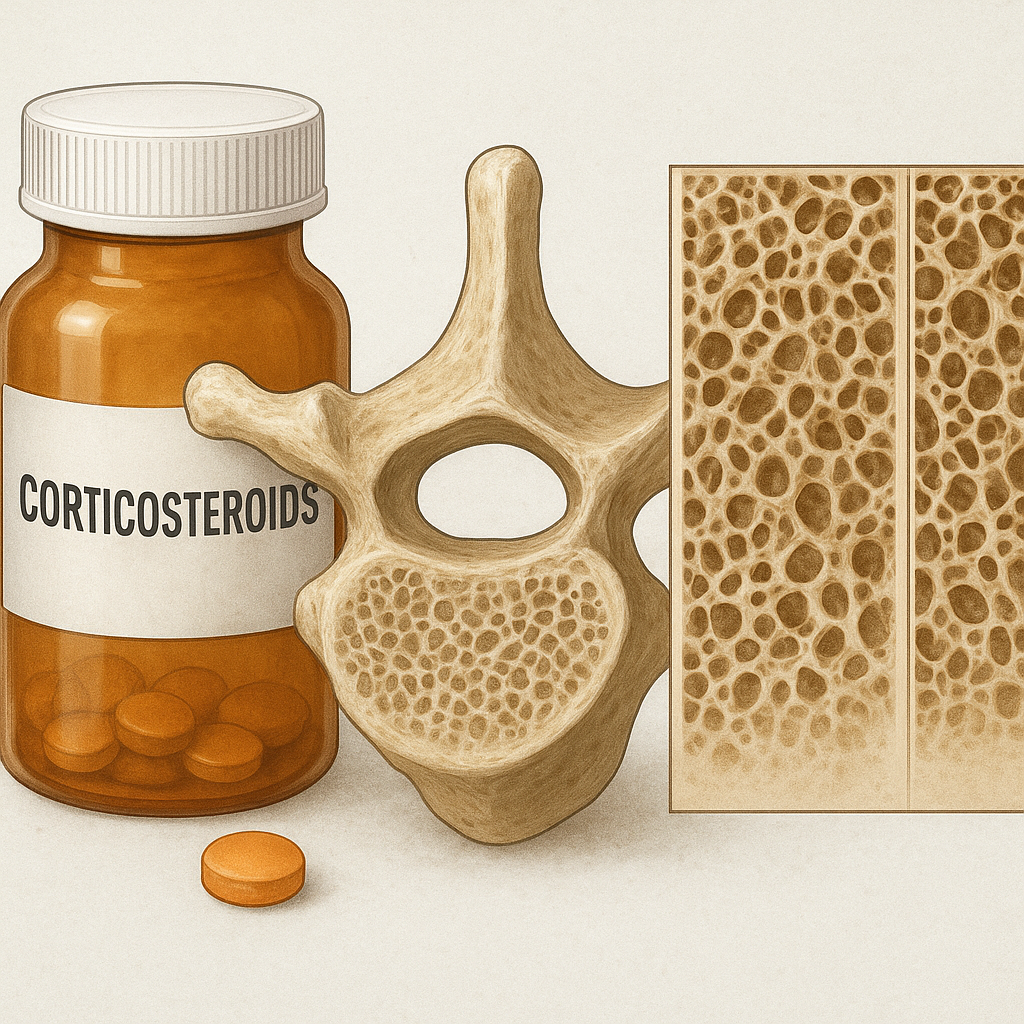
The pervasive use of corticosteroids in modern medicine has revolutionized the management of numerous inflammatory and autoimmune conditions. However, the widespread prescription of these agents has brought to light significant concerns about their impact on bone mineral density and overall skeletal health. This article explores the multifaceted ways in which corticosteroids affect bone metabolism, clinical consequences of long-term therapy, associated risk factors, and potential strategies to mitigate adverse outcomes.
Mechanisms of Corticosteroid Action on Bone Metabolism
Corticosteroids, particularly glucocorticoids, exert profound effects on the cellular components of bone tissue. Understanding these mechanisms requires a close examination of how these drugs influence osteoblasts, osteoclasts, and the bone matrix.
Suppression of Bone Formation
Corticosteroids diminish the number and functionality of osteoblasts, the cells responsible for synthesizing new bone. They achieve this by:
- Reducing proliferation and differentiation of osteoprogenitor cells.
- Inhibiting expression of key transcription factors such as Runx2.
- Promoting apoptosis of mature osteoblasts through upregulation of pro-apoptotic proteins.
Moreover, corticosteroids interfere with the production of collagen, the primary organic component of the bone matrix, thus weakening bone strength and resilience.
Enhanced Bone Resorption
While inhibiting bone formation, corticosteroids concurrently stimulate the activity of osteoclasts, cells that break down bone tissue. This dual action accelerates bone loss by:
- Increasing expression of RANKL (Receptor Activator of Nuclear factor Kappa-Β Ligand) on osteoblasts and stromal cells.
- Decreasing production of OPG (Osteoprotegerin), a decoy receptor that normally binds RANKL to limit osteoclastogenesis.
- Modulating the balance of cytokines such as interleukin-1 and tumor necrosis factor-alpha to favor bone resorption.
Impaired Calcium Homeostasis
Corticosteroids reduce calcium absorption in the gastrointestinal tract and increase renal excretion of calcium. The resulting hypocalcemia triggers a compensatory rise in parathyroid hormone (PTH), which further enhances bone resorption. Chronic alterations in calcium balance contribute significantly to decreased bone density.
Clinical Consequences of Long-Term Corticosteroid Therapy
Long-term or high-dose corticosteroid therapy has been consistently associated with an elevated risk of osteoporosis and bone fractures. The clinical picture can vary depending on dosage, duration, and patient-specific factors.
Incidence of Steroid-Induced Osteoporosis
Studies indicate that up to 50% of patients receiving daily doses equivalent to 7.5 mg of prednisone for longer than six months develop osteoporosis. The greatest bone loss occurs within the first six months of therapy, with an annual decline in bone mineral density of 2–3% at the lumbar spine and hip regions.
Fracture Risk and Morbidity
Fractures related to corticosteroid use can occur even in the absence of significant drops in bone density. Vertebral compression fractures are particularly common and may present with sudden back pain, height loss, or kyphosis. Peripheral fractures of the wrist and hip also contribute to increased morbidity and reduced quality of life.
Risk Factors and Prevention Strategies
Not all patients on corticosteroid therapy will develop severe bone loss. Identifying modifiable and non-modifiable risk factors can guide personalized prevention approaches.
Non-Modifiable Risk Factors
- Advanced age
- Female sex, particularly postmenopausal status
- Family history of osteoporosis or fragility fracture
- Low baseline bone mineral density
Modifiable Risk Factors
- Smoking and excessive alcohol consumption
- Physical inactivity
- Poor nutritional intake, especially inadequate calcium and vitamin D
- Concomitant use of medications such as proton pump inhibitors or anticonvulsants
Preventive Measures
- Baseline and periodic assessment of bone mineral density via DXA scans.
- Optimizing calcium intake (1,000–1,200 mg daily) through diet or supplements.
- Ensuring adequate vitamin D levels (25-hydroxyvitamin D >30 ng/mL).
- Encouraging weight-bearing and muscle-strengthening exercise.
- Implementing lifestyle changes such as smoking cessation and moderation of alcohol.
Therapeutic Approaches and Future Directions
Preventing and treating corticosteroid-induced bone loss involves a multidisciplinary strategy that includes pharmacologic agents, lifestyle modification, and emerging therapies.
Pharmacologic Interventions
- Bisphosphonates: First-line agents that inhibit osteoclast-mediated bone resorption. Examples include alendronate and risedronate.
- Denosumab: A monoclonal antibody against RANKL that effectively reduces bone turnover.
- Teriparatide: Recombinant PTH analog that stimulates osteoblast activity and bone formation.
- SERMs (Selective Estrogen Receptor Modulators): Such as raloxifene, used primarily in postmenopausal women.
- Calcitonin: Less potent but can provide analgesic benefit in acute vertebral fractures.
Emerging Therapies
Novel agents under investigation aim to more precisely target the molecular pathways disrupted by corticosteroids. These include:
- Wnt signaling modulators to enhance osteoblastogenesis.
- Anti-sclerostin antibodies to promote bone formation.
- Gene therapy approaches to rectify imbalances in cytokine expression.
Interdisciplinary Care Model
Optimal management of patients on long-term corticosteroids requires collaboration between endocrinologists, rheumatologists, primary care physicians, and nutritionists. Regular monitoring, patient education, and timely initiation of preventive therapy can significantly reduce the burden of steroid-induced bone disease.
Conclusion
While corticosteroids remain indispensable in managing many serious conditions, their negative impact on skeletal health cannot be overlooked. By elucidating the complex mechanisms by which these drugs interfere with bone metabolism and implementing comprehensive prevention and treatment strategies, healthcare providers can mitigate the risk of osteoporosis and fractures, preserving patient mobility and quality of life.