Chronic inflammation is a persistent immune response that can profoundly alter the health and integrity of the skeletal system. While acute inflammatory reactions serve to protect the body from injury and infection, long-term immune activation can disrupt the delicate balance of bone metabolism, leading to increased fragility and risk of fracture. Understanding how sustained inflammatory signals influence bone cells and tissue architecture is vital for developing targeted approaches to preserve bone health in patients with autoimmune disorders, chronic infections, and metabolic syndromes.
The Mechanisms Linking Chronic Inflammation to Bone Loss
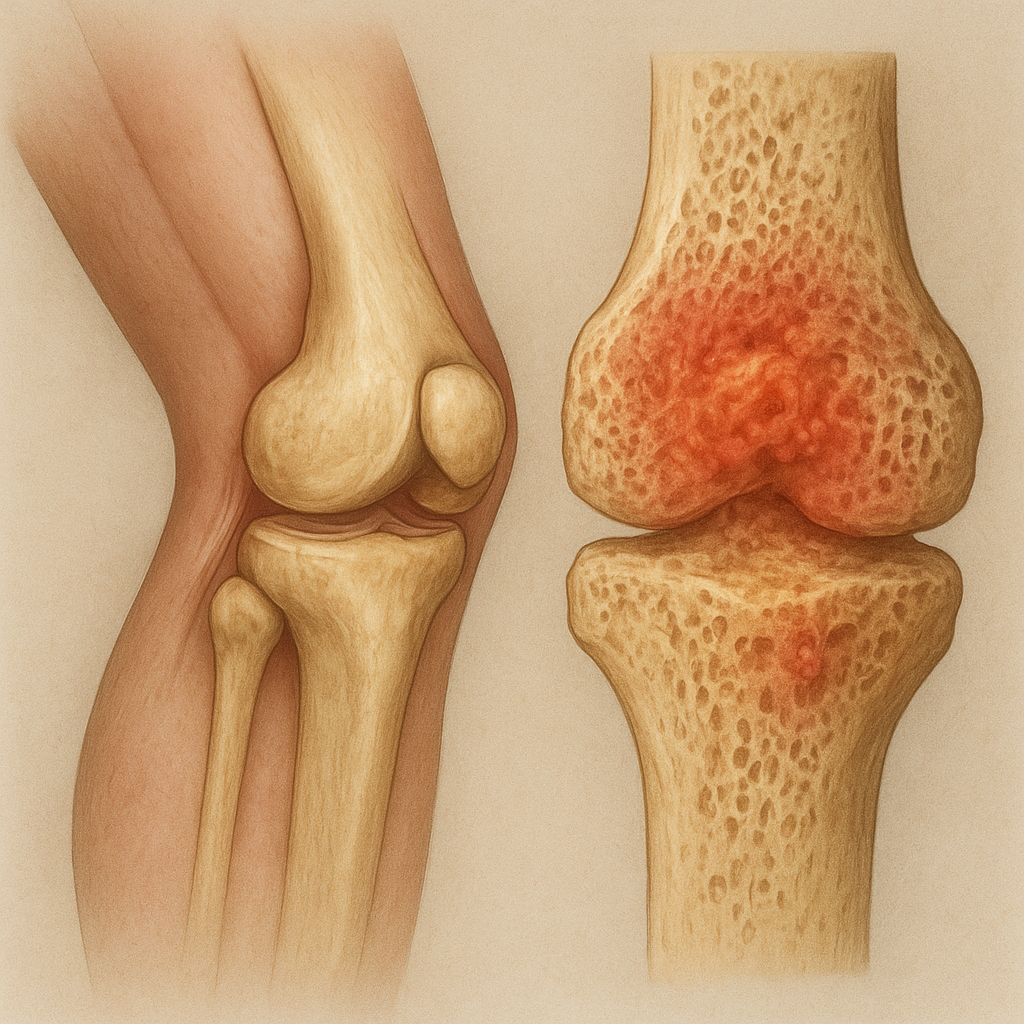
At the cellular level, bone remodeling is orchestrated by two primary cell types: osteoclasts, responsible for bone resorption, and osteoblasts, which drive bone formation. Under normal conditions, these activities are tightly coupled, ensuring skeletal strength and mineral homeostasis. However, a persistent inflammatory environment disrupts this equilibrium through several intertwined mechanisms.
Cytokine Milieu and Cellular Cross-talk
Pro-inflammatory cytokines such as interleukin-1 (IL-1), tumor necrosis factor-alpha (TNF-α), and interleukin-6 (IL-6) create a hostile cytokine milieu in the bone microenvironment. These signaling molecules:
- Enhance osteoclast activity by upregulating receptor activator of nuclear factor κB ligand (RANKL) expression on stromal cells and osteoblast precursors.
- Inhibit osteoblast differentiation via downregulation of osteogenic transcription factors such as Runx2 and osterix.
- Promote the survival of existing osteoclasts and prolong their bone-resorbing lifespan.
As a result, the decoupled remodeling cycle favors net bone degradation, leading to reduced bone density and microarchitectural deterioration.
Oxidative Stress and Extracellular Matrix Damage
Chronic inflammation generates reactive oxygen species (ROS) and nitrogen species, inflicting oxidative damage on the bone extracellular matrix. ROS can degrade collagen fibers, impair mineral deposition, and trigger apoptosis in bone-forming cells. This oxidative assault compounds the effects of overactive osteoclasts, creating zones of structural weakness that predispose to microfractures and cortical thinning.
Clinical Consequences of Persistent Inflammatory States
Many chronic diseases feature an inflammatory component that directly impacts skeletal health. Recognizing these links is crucial for early intervention and risk stratification.
Rheumatoid Arthritis and Systemic Autoimmune Disorders
In conditions like rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), synovial inflammation spills into adjacent bone, accelerating joint erosion and periarticular bone loss. Beyond local effects, systemic cytokine overproduction fosters generalized osteoporosis. Patients with long-standing RA exhibit a twofold increase in fracture risk compared to healthy controls, underscoring the importance of integrated rheumatologic and orthopedic care.
Inflammatory Bowel Disease and Gut–Bone Axis
Inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis are associated with malabsorption of key minerals and vitamins, compounding immune-mediated bone loss. Elevated levels of TNF-α and IL-6 in the gastrointestinal tract can exert endocrine-like effects on distant bone cells. In addition, long-term corticosteroid therapy, commonly used to manage IBD flares, further undermines bone density by inhibiting osteoblastogenesis and reducing calcium absorption.
Metabolic Syndrome and Low-Grade Inflammation
Obesity and type 2 diabetes mellitus often present with a state of chronic low-grade inflammation. Adipose tissue secretes adipokines such as leptin, resistin, and adiponectin, which modulate immune responses and influence bone turnover. Although some studies suggest higher body mass may protect against fractures by biomechanical loading, the inflammatory component can offset these benefits, leading to impaired bone quality and increased fracture severity.
Innovative Strategies for Diagnosis and Management
Tackling inflammation-induced bone loss requires a multifaceted approach that addresses both the underlying immune dysregulation and the skeletal consequences. Emerging modalities focus on early detection, targeted therapy, and lifestyle optimization.
Advanced Biomarkers and Imaging Techniques
Traditional bone mineral density (BMD) assessment via dual-energy X-ray absorptiometry (DXA) provides a snapshot of skeletal mass but falls short of detecting active inflammatory damage. Novel biomarkers under investigation include serum levels of C-terminal telopeptide (CTX) for bone resorption, procollagen type 1 N-terminal propeptide (P1NP) for bone formation, and inflammatory mediators such as high-sensitivity C-reactive protein (hs-CRP) and IL-6. Meanwhile, high-resolution peripheral quantitative computed tomography (HR-pQCT) and magnetic resonance imaging (MRI) allow visualization of microarchitectural changes and local edema, enabling earlier intervention before gross bone loss occurs.
Targeted Pharmacotherapy
Biologic agents that neutralize specific cytokines have revolutionized the treatment of autoimmune disease and, by extension, mitigated their skeletal impact. Anti-TNF therapies (e.g., infliximab, adalimumab), IL-6 receptor antagonists (e.g., tocilizumab), and RANKL inhibitors (e.g., denosumab) directly attenuate inflammatory bone resorption. In addition, bisphosphonates remain a cornerstone for preventing fracture in high-risk individuals by inducing osteoclast apoptosis. The choice and timing of these agents must be personalized based on disease activity, fracture history, and comorbid conditions.
Immunomodulatory and Nutritional Interventions
Beyond pharmaceuticals, several lifestyle and dietary strategies can modulate the inflammatory milieu and support bone health:
- Regular weight-bearing exercise to stimulate osteoblast function and enhance mechanical strength.
- Dietary optimization with adequate calcium, vitamin D, and omega-3 fatty acids to reduce cytokine production and promote mineralization.
- Supplementation with probiotics and prebiotics, targeting the gut–bone axis to limit systemic inflammation.
- Stress reduction techniques such as mindfulness and yoga to lower cortisol levels and downstream inflammatory cascades.
Future Directions in Research and Clinical Practice
Efforts to unravel the intricate dialogue between the immune system and the skeleton continue to accelerate. Cutting-edge areas of investigation include:
- Gene-editing approaches to correct mutations in inflammatory mediators or bone regulatory genes.
- Cell-based therapies harnessing mesenchymal stem cells for immunomodulation and bone regeneration.
- Next-generation sequencing of the bone marrow microenvironment to identify novel biomarkers and therapeutic targets.
- Integration of artificial intelligence in imaging analysis for earlier detection of subclinical bone damage.
By bridging basic science discoveries with clinical applications, the goal is to preserve skeletal integrity in patients suffering from chronic inflammatory diseases and to reduce the global burden of fracture-related morbidity.