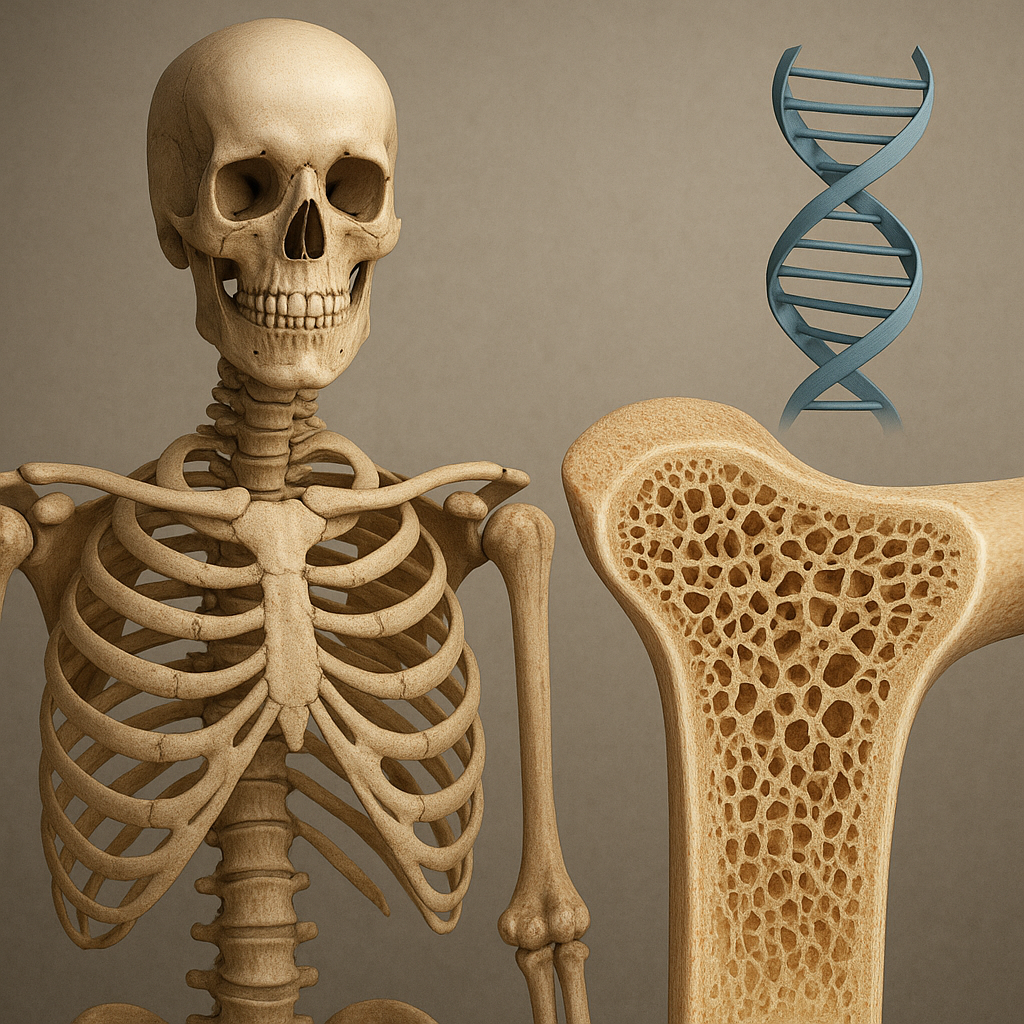
The interplay between heredity and skeletal integrity has garnered increasing attention as research unveils the complex genetic networks that govern bone formation, maintenance, and repair. This article explores how variations in our DNA shape the vulnerability to various bone conditions, from brittle bone syndromes to age-related degeneration. By examining critical gene pathways, examining inherited disorders, and highlighting innovative diagnostic and therapeutic strategies, we reveal the burgeoning impact of genomics on the field of orthopedics and endocrinology.
Genetic Foundations of Bone Health
Bones are dynamic organs, continuously remodeling in response to mechanical stress and metabolic demands. Central to this process are osteoblasts, osteoclasts, and osteocytes, whose functions are orchestrated by a network of signaling molecules and structural proteins. At the heart of healthy bone physiology lie genes that direct the synthesis of key components such as type I collagen, extracellular matrix proteins, and regulators of mineralization. Disruptions in these genetic instructions often manifest as altered bone density, reduced structural resilience, or improper mineral deposition.
Mechanisms of genetic control include:
- Transcription factors (e.g., RUNX2, SOX9) that activate or suppress bone-specific genes.
- Growth factors such as bone morphogenetic proteins (BMPs) that initiate osteogenesis.
- Receptor signaling pathways (e.g., RANK/RANKL/OPG) regulating osteoclast activity and resorption.
- Ion channels and transporters managing calcium homeostasis.
Mutations in any component of these pathways can lead to quantitative or qualitative defects in bone matrix and compromise mechanical properties.
Inherited Bone Disorders and Their Mechanisms
Several well-characterized syndromes illustrate how single-gene defects translate into clinical bone pathology. While some disorders present in early childhood, others emerge later, underscoring the varied expressivity of genetic variations.
Osteogenesis Imperfecta
Often termed “brittle bone disease,” osteogenesis imperfecta (OI) is most frequently caused by mutations in COL1A1 or COL1A2, genes encoding collagen type I. These mutations disrupt triple-helix formation, leading to bones that fracture with minimal trauma. Clinical manifestations range from mild forms to perinatal lethality, and extra-skeletal features can include dentinogenesis imperfecta and hearing loss.
Osteopetrosis
This rare condition is characterized by impaired osteoclast function, resulting in dense but fragile bones. Mutations in genes like TCIRG1, CLCN7, and CA2 affect acidification within osteoclast resorption lacunae. Patients often experience cranial nerve compression and hematopoietic insufficiency due to narrowed marrow cavities.
Hypophosphatasia
A deficiency of tissue-nonspecific alkaline phosphatase (TNSALP) leads to defective mineralization. Caused by mutations in the ALPL gene, hypophosphatasia presents a spectrum from perinatal lethal forms to late-onset stress fractures, dental anomalies, and musculoskeletal pain.
Genetic Risk Factors for Common Conditions
- Osteoporosis: Polygenic contributions involve genes regulating estrogen receptors, vitamin D metabolism, and Wnt signaling (e.g., LRP5).
- Paget’s disease of bone: Mutations in SQSTM1 alter osteoclastogenesis and lead to excessive bone turnover.
- Early-onset arthritis: Variants in COL2A1 and other cartilage matrix genes predispose to degenerative joint disease.
Technological Advances in Diagnosis
Accurate and early detection of genetic bone disorders is crucial for optimal management. Innovations in genomic technologies and imaging have revolutionized diagnostic capabilities.
- Genome sequencing: Whole-exome sequencing identifies both known and novel mutations in bone-related genes, enabling precise molecular diagnosis.
- Targeted gene panels: Focused panels for collagen disorders or osteoclast dysfunction expedite diagnosis with reduced costs.
- Biomarker assays: Circulating levels of bone turnover markers, such as P1NP and CTX, complement genetic data in assessing disease activity.
- Advanced imaging: High-resolution peripheral quantitative CT (HR-pQCT) visualizes microarchitecture changes undetectable by dual-energy X-ray absorptiometry (DXA).
Coupling genetic data with clinical phenotypes allows for improved prognostication and personalized care plans.
Targeted Therapies and Future Prospects
Understanding the molecular basis of bone disorders paves the way for precision medicine. In recent years, several promising interventions have emerged.
- Bisphosphonates and denosumab: Anti-resorptive agents that inhibit osteoclasts, providing fracture risk reduction in osteoporosis and OI.
- Enzyme replacement therapy: Asfotase alfa for hypophosphatasia supplements deficient alkaline phosphatase, improving survival and skeletal outcomes.
- Gene therapy: Experimental approaches aim to correct or silence pathogenic mutations. Viral vectors delivering functional COL1A1 genes have shown efficacy in animal models of OI.
- CRISPR/Cas9 genome editing: Preclinical studies demonstrate the potential to repair mutations in situ, offering a permanent cure for monogenic bone diseases.
Emerging research in mechanotransduction and the role of microRNAs as regulatory biomarkers promises further breakthroughs. Combining biochemical, genetic, and biomechanical insights may soon yield novel agents that stimulate bone formation rather than merely inhibit resorption.
Ethical, Social, and Regulatory Considerations
With the advent of gene-based interventions, ethical questions arise regarding germline editing, equitable access to costly therapies, and long-term safety. Regulatory frameworks must evolve to address these challenges, ensuring responsible translation from bench to bedside.
- Informed consent complexities for prenatal or pediatric gene editing.
- Health disparities in accessing advanced genomic testing.
- Post-marketing surveillance for unforeseen adverse events of gene therapies.
Collaborations between clinicians, genetic counselors, policymakers, and patient advocates are essential to navigate these multifaceted issues.
Concluding Remarks
The genetic underpinnings of bone disorders illuminate both fundamental aspects of skeletal biology and pathways for therapeutic innovation. As genomic technologies become more accessible and safe editing techniques evolve, the prospect of preventing or reversing debilitating bone diseases moves closer to reality. Interdisciplinary efforts will remain critical in harnessing the full potential of genetics to improve musculoskeletal health for future generations.