The process of bone regeneration is governed by multiple biological pathways, each stage crucial for achieving full structural and functional recovery. Interruptions or delays in this sequence can compromise the final outcome, making accurate, timely evaluation essential. Radiographic tools offer noninvasive windows into the internal microarchitecture and dynamic patterns of tissue growth. From conventional X-rays to state-of-the-art imaging systems, clinicians and researchers can now apply a spectrum of diagnostics to monitor progress and predict long-term success.
Fundamentals of Bone Healing
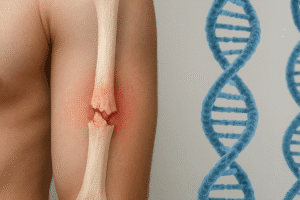
After a fracture or surgical osteotomy, the skeleton initiates a tightly orchestrated repair program. This cascade spans immediate inflammatory responses to gradual tissue remodeling. A clear grasp of each segment allows for better interpretation of images, as distinct radiographic features correspond to specific biological events.
Biological Phases and Radiographic Signatures
- Inflammatory Phase – Hematoma formation and inflammatory cell infiltration.
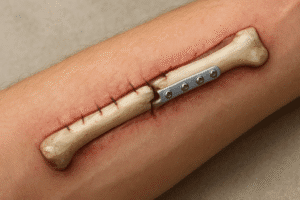
- Repair Phase – Soft callus formation, followed by mineralized callus bridging the defect.
- Remodeling Phase – Conversion of woven bone into lamellar bone, restoring original contour.
During the initial inflammatory period, plain radiographs often reveal widening of the fracture line without appreciable mineralization. As callus tissue emerges, increases in local opacity mark the onset of osteogenesis. Finally, the remodeling phase is characterized by gradual smoothing of the callus and restoration of normal cortical outlines.
Principles of Radiographic Evaluation
Choosing the proper imaging strategy depends on defect location, patient factors, and the specific information required. Standard radiographs remain the workhorse in orthopedic practice, while cross-sectional techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) deliver enhanced detail.
Plain Radiography
Traditional X-rays provide rapid, cost-effective snapshots of gross alignment and mineralization patterns. Key parameters include:
- Fracture alignment and angulation
- Extent of cortical disruption
- Presence and density of periosteal callus
Sequential radiographs taken at defined intervals enable clinicians to create a timeline of healing. Variations in bone density and callus size can be quantified by grayscale analysis in digital radiography platforms, adding a quantitative element to what was once a purely qualitative assessment.
Computed Tomography and MRI
CT imaging offers high-resolution volumetric data, ideal for evaluating complex fractures or nonunions. It permits 3D reconstruction of the defect and precise measurement of density in Hounsfield Units (HU), which correlates with mineral content.
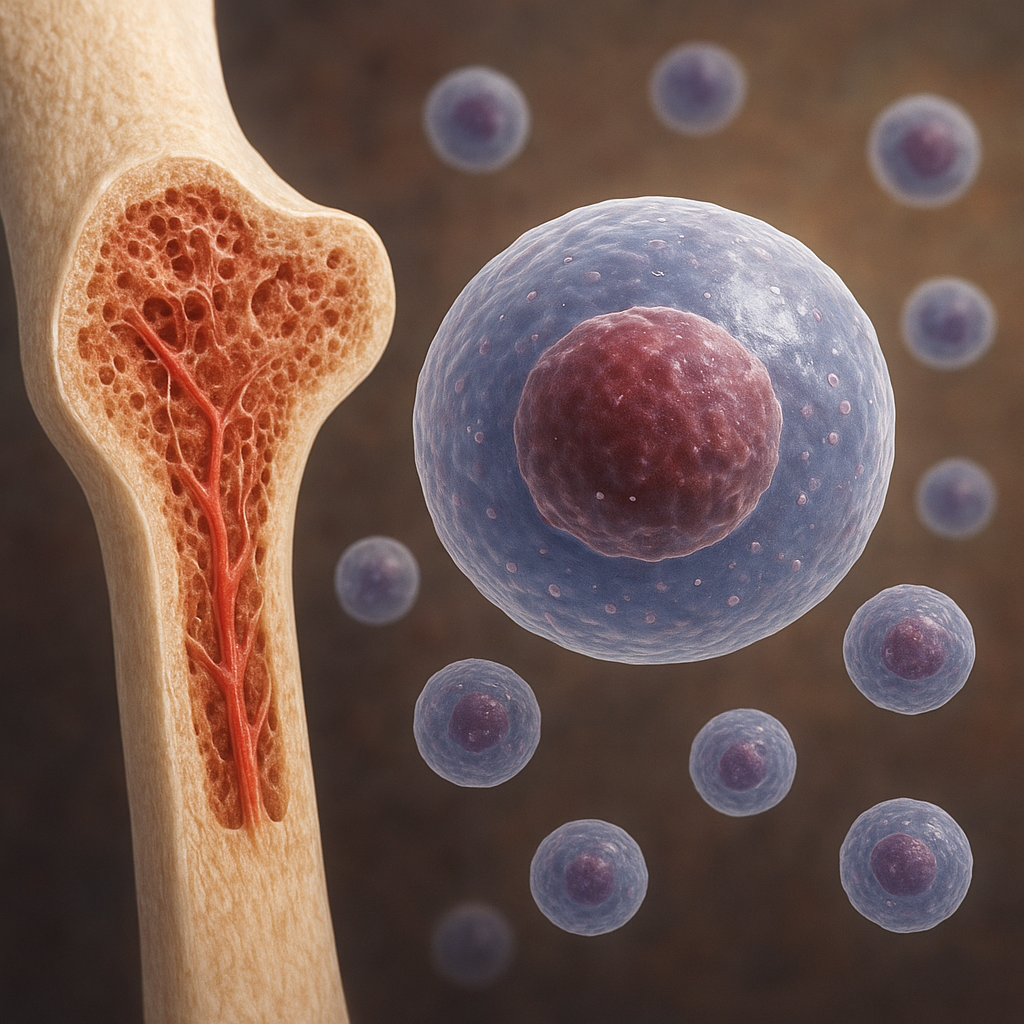
MRI excels at visualizing soft tissue and vascularity around the healing site. T2-weighted sequences can reveal edema or fluid collection, while T1 sequences display bone marrow conversion patterns. Contrast-enhanced MRI may highlight areas of active osteogenesis through increased perfusion.
Advanced Imaging Modalities and Innovations
Beyond standard tomographic scans, emerging techniques are broadening the diagnostic landscape. These tools not only track structural changes but also probe metabolic and molecular processes within the repair tissue.
Ultrasound Elastography
Ultrasound offers a radiation-free alternative for bedside monitoring. Elastography maps mechanical stiffness, distinguishing soft callus from mineralized tissue. Serial studies can track the transition from pliable fibrous tissue to rigid bone, aiding in early detection of delayed unions.
Nuclear Medicine and PET/SPECT
Positron emission tomography (PET) and single photon emission computed tomography (SPECT) utilize radiotracers that localize to areas of high osteoblastic activity. When fused with CT, these scans reveal hotspots of healing at the cellular level, supporting decisions on weight-bearing progression or adjuvant therapies.
Optical and Spectroscopic Methods
Near-infrared spectroscopy and Raman scattering techniques show promise for assessing bone composition in vivo. These methods detect variations in mineral-to-matrix ratios, offering insight into the maturation state of the callus without ionizing radiation.
Quantitative Assessment and Clinical Applications
Clinicians require standardized metrics to compare outcomes across patients and studies. Various scoring systems and software tools now extract objective markers from image data, guiding treatment algorithms.
Scoring Systems and Indices
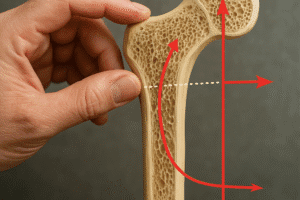
- Radiographic Union Score for Tibial Fractures (RUST) – Evaluates cortical bridging on four cortices.
- Lane and Sandhu Score – Rates callus volume and union quality on a 5-point scale.
- Radiographic Union Scale for Hip (RUSH) – Adapts RUST criteria for proximal femur evaluations.
Each index translates visual cues into numerical values, facilitating research comparisons and predictive modeling. Studies correlating early score improvements with final functional outcomes underscore the prognostic power of these tools.
Software-Driven Analytics and Machine Learning
Artificial intelligence algorithms analyze large datasets of radiographs and cross-sectional images to identify patterns invisible to the human eye. Deep learning models have been trained to detect subtle textural changes in trabecular bone, accelerating the identification of union failure risks. Integration with electronic health records enables real-time alerts when healing deviates from expected trajectories.
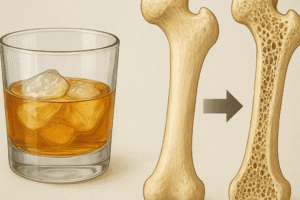
Clinical Decision-Making and Patient Management
Accurate, timely imaging reassures both patient and surgeon that recovery is on track. Delays in union may prompt interventions such as bone grafting, pharmacotherapy with anabolic agents, or mechanical stimulation. Conversely, radiographic evidence of robust callus formation can fast-track rehabilitation protocols and reduce immobilization time.
Future Directions and Research Opportunities
Ongoing investigations aim to refine imaging biomarkers and deliver even more personalized care. Molecular probes targeting specific osteogenic pathways could allow real-time visualization of receptor activity. Likewise, integration of wearable sensors and point-of-care ultrasound promises continuous monitoring outside the clinic, a paradigm shift in post-operative follow-up.
As technology advances, the synergy of biological science and imaging innovation will continue to enhance our capacity to evaluate and optimize modalities for bone regeneration. The ultimate goal remains unobstructed: restore the integrity of skeletal structures with minimal patient burden, driven by data-informed strategies and a deep understanding of the healing journey.