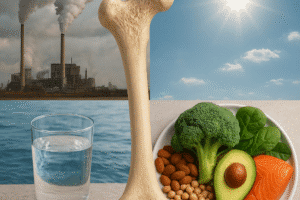
Calcium plays a pivotal role in maintaining bone integrity and proper physiological processes throughout the human body. While dietary sources often meet daily requirements, many individuals turn to supplementation to ensure adequate intake. This article explores the intricate relationship between calcium and skeletal health, addresses the potential benefits of supplements, and examines the risks associated with overconsumption. By understanding the interplay between nutrition, metabolic pathways, and individual needs, readers can make informed decisions regarding optimal strategies for supporting lifelong skeletal strength.
Understanding Calcium and Skeletal Health
The Role of Calcium in the Body
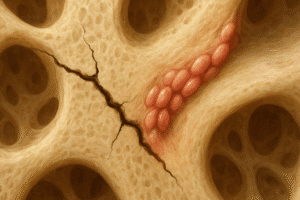
Calcium is the most abundant mineral in the human body, with approximately 99% stored in the bone matrix. It contributes to skeletal rigidity by forming hydroxyapatite crystals in bone tissue, which confers mechanical strength and structural stability. Beyond the skeleton, calcium ions participate in blood clotting, muscle contraction, nerve conduction, and hormonal secretion. Proper regulation of serum calcium is critical: when dietary intake falls short, the body mobilizes calcium from the bone reservoir, potentially compromising skeletal integrity over time.
Absorption and Metabolism of Calcium
Dietary calcium is primarily absorbed in the small intestine through active and passive mechanisms. Vitamin D plays a central role by upregulating transport proteins that facilitate absorption across enterocytes. Factors influencing absorption efficiency include:
- Age and hormonal status (e.g., menopause reduces estrogen levels, impairing calcium uptake).
- Presence of dietary inhibitors such as oxalates, phytates, and excessive dietary fat.
- Concurrent intake of other minerals like magnesium and phosphorus, which compete for transport.
- Vitamin D status and overall gastrointestinal health.
Understanding these determinants helps tailor nutrition plans and supplement regimens for maximal benefit.
Benefits of Calcium Supplementation
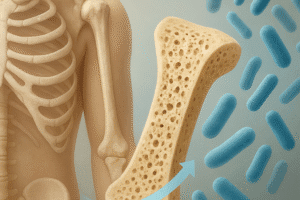
Prevention and Management of Osteoporosis
Osteoporosis, characterized by reduced bone mass and microarchitectural deterioration, increases fracture risk in older adults. Adequate calcium intake, combined with vitamin D, forms the cornerstone of osteoporosis prevention and management. Clinical trials demonstrate that daily supplementation can slow bone loss in postmenopausal women and elderly men, reducing incidence of vertebral and hip fractures. While supplements cannot fully reverse established disease, they play a valuable role in maintaining peak bone mass and mitigating age-related decline.
Support for Bone Mineral Density in At-Risk Populations
Certain groups may benefit particularly from supplementation due to increased requirements or impaired absorption:
- Postmenopausal women with estrogen deficiency.
- Individuals on long-term corticosteroid therapy, which accelerates bone resorption.
- People with gastrointestinal disorders (e.g., celiac disease, inflammatory bowel disease).
- Vegans and lactose-intolerant individuals with limited dietary calcium sources.
- Athletes with high sweat losses or female athletes with menstrual irregularities.
By addressing gaps in dietary calcium, supplements help maintain skeletal resilience during periods of heightened vulnerability.
Potential Risks and Precautions
Cardiovascular and Renal Considerations
Concerns have emerged regarding high-dose calcium supplements and cardiovascular events. Some observational studies link supplemental calcium to increased risk of myocardial infarction and stroke, possibly due to transient elevations in serum calcium leading to vascular calcification. However, results remain mixed, and the risk appears negligible when calcium is obtained through food sources. Additionally, excessive calcium intake can contribute to nephrolithiasis by increasing urinary calcium excretion, particularly in susceptible individuals.
Gastrointestinal Side Effects
Common adverse effects of calcium supplements include:
- Constipation
- Bloating and gas
- Abdominal cramping
Dividing the total daily dose into smaller administrations and selecting formulations (e.g., calcium citrate vs. carbonate) based on individual tolerance can alleviate discomfort.
Guidelines for Optimal Calcium Intake
Recommended Dietary Allowances and Upper Limits
Health authorities generally recommend the following average daily calcium intakes:
- Adolescents (9–18 years): 1,300 mg
- Adults (19–50 years): 1,000 mg
- Women (51+ years) and men (71+ years): 1,200 mg
The tolerable upper intake level is set at 2,500 mg for adults under 50 and 2,000 mg for those over 50. Exceeding these thresholds increases the likelihood of risks such as renal complications and potential vascular calcification.
Strategies to Maximize Calcium Bioavailability
Combining calcium supplements with meals enhances absorption by leveraging the acidic environment required to solubilize calcium salts. Adequate vitamin D status (serum 25-hydroxyvitamin D above 20 ng/mL) is imperative. Weight-bearing exercise further stimulates osteoblastic activity and promotes deposition of dietary calcium into the bone matrix. Moreover, moderating sodium intake and maintaining a diet rich in fruits and vegetables supports a favorable acid-base balance for skeletal health.
Personalizing Supplemental Regimens
Decisions about calcium supplementation should consider:
- Baseline dietary calcium intake
- Individual risk factors for osteoporosis and fractures
- Coexisting medical conditions (e.g., kidney disease, hyperparathyroidism)
- Potential drug-nutrient interactions (e.g., with bisphosphonates, thyroid hormone)
Consultation with healthcare professionals allows for tailored dose adjustments, monitoring of serum calcium levels, and integration of lifestyle modifications to optimize outcomes.