Bone resorption is a finely tuned physiological process essential for maintaining skeletal integrity and adapting to mechanical stress. In health, this dynamic balance between degradation and formation preserves optimal bone density and structural resilience. Disruption of this equilibrium, however, can lead to excessive bone loss, contributing to osteoporosis, metabolic bone diseases, and heightened fracture risk. Insights into the cellular machinery and molecular signals driving bone resorption have paved the way for targeted therapeutic interventions. This article explores the core mechanisms, pathological alterations, and current as well as emerging treatment strategies.
Physiology of Bone Remodeling
Skeletal homeostasis relies on continuous remodeling carried out by coordinated actions of bone-resorbing cells and bone-forming cells. During each remodeling cycle, microdamage induced by fatigue loading is detected and removed, while new mineralized matrix is deposited.
Cellular Players
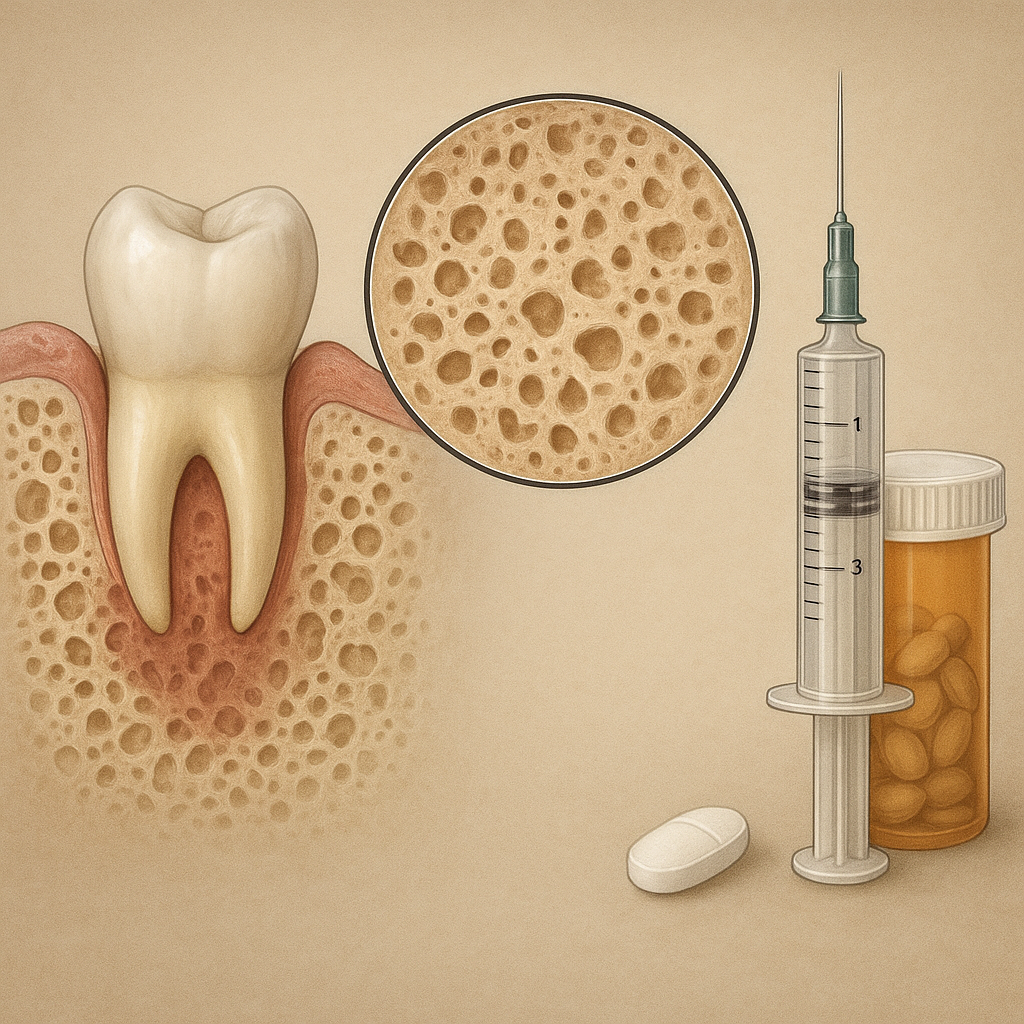
Osteoclasts are specialized multinucleated cells responsible for matrix degradation. Originating from hematopoietic precursors, they attach to the bone surface, form a sealed resorption lacuna, and secrete protons and proteolytic enzymes. Conversely, osteoblasts, derived from mesenchymal stem cells, synthesize collagen-rich osteoid and initiate mineralization. The tight coupling of these two cell types ensures that resorption sites are rapidly refilled, preventing net bone loss under physiological conditions.
Molecular Signaling: RANKL/OPG Pathway
The receptor activator of nuclear factor kappa-Β ligand (RANKL) and its decoy receptor osteoprotegerin (OPG) are central regulators of osteoclastogenesis. Stromal cells and osteoblast-lineage cells express RANKL, which binds to RANK on osteoclast precursors, promoting differentiation and activation. OPG sequesters RANKL, inhibiting its interaction with RANK and thus restraining resorption. The relative concentrations of RANKL and OPG in the bone microenvironment dictate the rate of osteoclast formation and activity. Additional modulators include macrophage-colony stimulating factor (M-CSF) and various cytokines that fine-tune this balance.
Mechanisms of Pathological Bone Resorption
Alterations in the regulatory networks of remodeling can shift the balance toward excessive resorption. Chronic inflammation, hormonal changes, genetic predispositions, and metabolic derangements all contribute to pathological bone loss.
Inflammatory Factors and Cytokines
Proinflammatory mediators such as tumor necrosis factor-alpha (TNF-α), interleukin-1 (IL-1), and interleukin-6 (IL-6) amplify osteoclastic activity. These cytokines upregulate RANKL expression on stromal cells and diminish OPG production, creating a pro-resorptive environment. Conditions like rheumatoid arthritis exemplify how persistent inflammation accelerates bone erosion, leading to joint deformities and systemic osteoporosis.
Hormonal Influences
Endocrine factors impact bone remodeling profoundly. Estrogen deficiency post-menopause removes a key inhibitory signal on osteoclasts, resulting in heightened RANKL levels and rapid bone loss. Glucocorticoids, when used chronically, promote osteoblast apoptosis and enhance osteoclast survival, contributing to steroid-induced osteoporosis. Parathyroid hormone (PTH), in intermittent doses, has an anabolic effect, whereas sustained hyperparathyroidism increases resorption.
Genetic and Metabolic Disorders
Genomic mutations affecting signaling molecules or structural proteins can underlie rare bone diseases. For example, mutations in the gene encoding cathepsin K cause pycnodysostosis, characterized by impaired resorption and brittle skeletons. Conversely, genetic variants promoting excessive RANKL activity predispose individuals to early-onset osteoporosis. Metabolic dysfunction, including vitamin D deficiency and renal osteodystrophy, similarly disrupts mineral homeostasis and remodeling.
Current and Emerging Treatments
Interventions aim to restore balance by either inhibiting excessive resorption or stimulating bone formation. Advances in molecular biology have yielded targeted agents with improved efficacy and safety profiles.
Antiresorptive Agents
- Bisphosphonates: These synthetic analogues of pyrophosphate bind to hydroxyapatite and are internalized by osteoclasts, inducing apoptosis. Oral formulations like alendronate and intravenous options such as zoledronic acid effectively reduce fracture risk. However, long-term use warrants monitoring for atypical femoral fractures and osteonecrosis of the jaw. Bisphosphonates remain first-line in moderate to severe osteoporosis.
- Denosumab: A human monoclonal antibody against RANKL, denosumab potently inhibits osteoclast formation. Administered subcutaneously every six months, it achieves rapid declines in bone turnover markers. Its reversible action upon discontinuation necessitates transition strategies to prevent rebound resorption.
- Selective Estrogen Receptor Modulators: Agents such as raloxifene mimic estrogen’s protective effects on bone without endometrial stimulation, offering an alternative for postmenopausal women at risk of breast cancer.
Anabolic Therapies
- Teriparatide: Recombinant PTH (1–34), teriparatide given daily stimulates osteoblast activity and enhances bone microarchitecture. Reserved for high-risk individuals, its use is limited to two years due to theoretical risk of osteosarcoma observed in animal studies.
- Abaloparatide: A PTH-related peptide analog with similar anabolic properties, offering slightly improved tolerability in some patients.
- Sclerostin Inhibitors: Antibodies targeting sclerostin—a Wnt signaling antagonist produced by osteocytes—unlock potent bone-forming pathways. Romosozumab demonstrates both anabolic and antiresorptive effects, representing a novel dual-action approach.
Novel Targets and Strategies
Research continues to identify new molecular targets. Inhibitors of cathepsin K aim to block collagen degradation by osteoclasts while preserving bone formation signals. Gene therapy techniques, such as delivery of OPG or siRNA against proteolytic enzymes, hold promise but face delivery challenges. Tissue engineering incorporating scaffolds seeded with osteoprogenitor cells and growth factors seeks to repair critical-size defects in cases of severe bone loss.
Integration of Clinical Management
Optimal care for patients with excessive bone resorption demands a multidisciplinary approach. Assessment of fracture risk incorporates bone densitometry, biochemical markers of turnover, and evaluation of secondary causes. Lifestyle modifications including weight-bearing exercise, adequate calcium and vitamin D intake, smoking cessation, and fall prevention complement pharmacotherapy. Personalized treatment plans weigh factors such as comorbidities, patient preferences, and potential adverse effects. Emerging digital tools and biomarkers may soon allow real-time monitoring of treatment response, enabling dynamic adjustment of therapeutic regimens.
Future Directions
Advancements in genomics, proteomics, and cell biology continue to expand our understanding of bone biology. Novel imaging techniques, including high-resolution peripheral quantitative computed tomography, afford three-dimensional insights into microarchitectural changes. Machine learning algorithms analyzing large datasets may predict individual responses to therapy, guiding precision medicine. Ultimately, combining antiresorptive and anabolic agents in optimized sequences or developing single molecules with dual action could revolutionize treatment paradigms. Continued exploration of the skeletal niche, immune interactions, and mechanical regulation will reveal further targets to preserve skeletal health across the lifespan.