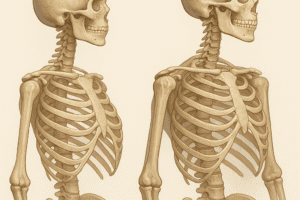
Bone regeneration represents a multifaceted challenge in orthopedics and regenerative medicine, demanding innovations that recapitulate native tissue architecture and biological signaling. Advances in material science have spurred the development of biomimetic constructs designed to direct cellular behavior, promote vascularization, and restore structural integrity. This article explores key aspects of designing, fabricating, and translating biomimetic materials for enhanced osteogenesis, focusing on scaffold architectures, bioactive cues, and preclinical to clinical pathways.
Design Principles of Biomimetic Materials
Engineering a successful bone substitute requires harmonizing multiple criteria that mimic the native extracellular matrix (ECM) and support the bone healing cascade. Core design principles include:
- Biocompatibility: Minimizing immune response and ensuring cytocompatibility with osteoblasts and mesenchymal stem cells.
- Degradation kinetics aligned with new tissue formation, avoiding premature collapse or prolonged presence.
- Osteoconduction and osteointegration, facilitating cellular infiltration and direct bonding between host tissue and implant.
- Mechanical properties tailored to match load-bearing requirements and avoid stress shielding.
- Incorporation of growth factors and cytokines for directed differentiation and angiogenic support.
Material selection often involves composites of ceramics, polymers, and bioactive glasses. For instance, blends of poly(lactic-co-glycolic acid) (PLGA) with hydroxyapatite nanoparticles yield tunable porosity and mechanical strength, while surface modifications with peptide sequences enhance cell adhesion.
Scaffold Architectures and Fabrication Techniques
Advanced fabrication technologies enable precise control over scaffold geometry, pore interconnectivity, and nanoscale features. Key approaches include:
Three-Dimensional (3D) Printing and Bioprinting
- Layer-by-layer deposition to create complex geometries closely matching patient-specific defects.
- Co-printing of living cells with biomaterials for in situ formation of cell-laden constructs.
- Integration of sacrificial inks to generate perfusable vascular channels.
Electrospinning and Nanofiber Scaffolds
- Fine fiber diameters (50–500 nm) mimic collagen fibrils, enhancing cell attachment and matrix deposition.
- Composite fibers incorporating bioactive ceramics to boost osteoconductivity.
- Aligned fibers guide cell orientation, influencing mechanical anisotropy and tissue organization.
Sol–Gel and Gas Foaming Techniques
- Sol–gel routes produce bioactive glass networks with tailored dissolution rates, releasing therapeutic ions.
- Gas foaming creates high-porosity scaffolds without high-temperature sintering, preserving growth factor bioactivity.
By integrating nanotechnology—such as surface nanotopographies or nanoparticle inclusion—researchers can further modulate protein adsorption and stem cell fate decisions, driving robust new tissue formation.
Bioactive Factors and Cellular Interactions
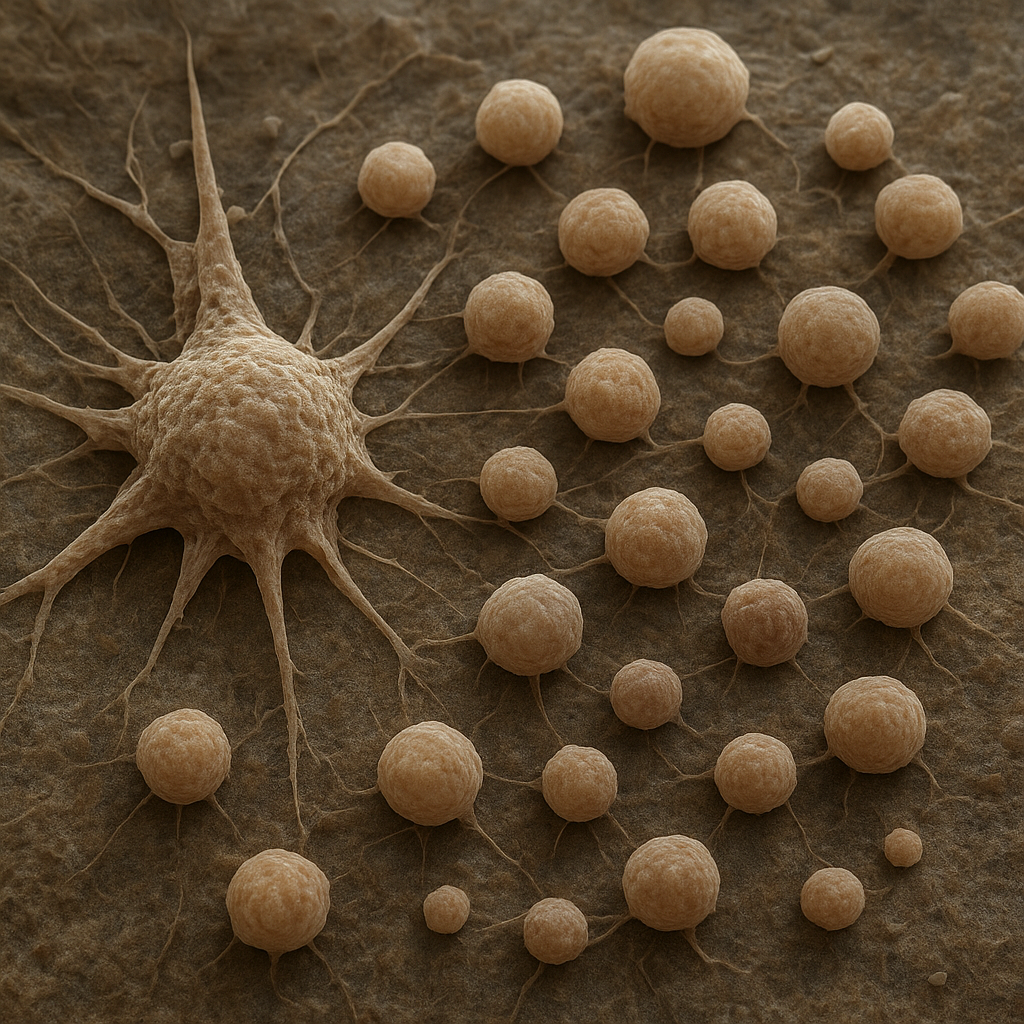
Beyond physical scaffolds, the orchestration of biological signals is paramount. Biomimetic constructs can carry a variety of cues:
- Growth factors (e.g., BMP-2, VEGF) delivered via controlled-release microspheres to promote angiogenesis and osteogenic differentiation.
- Peptide motifs (RGD, PHSRN) tethered to surfaces to enhance integrin-mediated adhesion.
- Gene delivery vectors encoding osteogenic transcription factors, enabling sustained local production of proteins.
- Exosome-loaded matrices to harness paracrine signaling for immune modulation and tissue repair.
Interactions between implanted materials and host cells proceed through integrin binding, cytoskeletal remodeling, and downstream signaling pathways such as Wnt/β-catenin. Optimizing the spatiotemporal presentation of these cues is essential to recapitulate the sequential phases of inflammation, proliferation, and remodeling that occur during natural bone healing.
Preclinical Models and Translational Challenges
Rigorous evaluation in animal models provides critical insights into performance, safety, and scalability of biomimetic materials. Commonly employed models include:
- Rodent critical-size calvarial defects for rapid screening of osteoconductive properties.
- Rabbit and canine segmental long-bone defects to assess load-bearing capacity and integration under mechanical stress.
- Large mammal (ovine, porcine) models for preclinical validation of surgical techniques and implant designs relevant to human anatomy.
Translational barriers often arise from differences in bone physiology, immune response, and scale. Regulatory pathways require comprehensive characterization of:
- Toxicology and immunogenicity profiles.
- Manufacturing reproducibility under good manufacturing practices (GMP).
- Long-term stability and degradation byproducts.
Moreover, cost-effectiveness and surgical workflow integration are critical for clinical adoption. Collaborative efforts between material scientists, surgeons, and regulatory bodies aim to streamline the path from bench to bedside.
Future Perspectives in Bone Tissue Engineering
Emerging trends in the field envision convergence of multiple disciplines to achieve truly functional bone regeneration:
- Smart biomaterials with responsive behavior, releasing bioactive agents upon mechanical loading or pH changes.
- Integration of patient-specific cells, including induced pluripotent stem cells (iPSCs), for personalized grafts.
- Advanced bioreactor systems for preconditioning constructs under dynamic mechanical and perfusion stimuli.
- Digital twins and computational modeling to predict in vivo performance and optimize implant design.
- Biofabrication of hierarchical structures that replicate Haversian systems and lacuno-canalicular networks.
As the landscape of regenerative medicine continues to evolve, interdisciplinary research will be pivotal in overcoming current limitations, ultimately providing robust solutions for complex bone defects and improving patient outcomes worldwide.