Bone marrow transplantation has revolutionized the treatment of multiple life-threatening disorders, offering a chance for cure in patients with leukemia, lymphoma, and various congenital immunodeficiencies. Over decades of research and clinical innovation, this procedure has evolved from experimental therapy into a **standard** of care in hematology and oncology. Its success hinges on precise biological mechanisms, including **hematopoietic** stem cell collection, **engraftment**, and immune modulation. This article explores the historical milestones, current innovations, and future directions in bone marrow **transplantation**, highlighting the critical interplay of science and patient care.
Origins and Evolution of Bone Marrow Transplants
The journey of bone marrow transplantation began in the mid-20th century, when investigators first recognized the marrow’s capacity to regenerate blood cell populations after lethal radiation exposure. Early experiments in mice paved the way for human trials in the 1950s. Landmark achievements include:
- 1956: First documented human transplant between identical twins, proving **stem cells** could reconstitute blood cell production.
- 1968: Introduction of **HLA** typing revolutionized donor-recipient **match** quality, significantly reducing rejection rates.
- 1975: Advances in immunosuppression enabled successful unrelated **donor** transplants.
- 1984: Recognition of graft-versus-tumor effect prompted integration of **graft-versus-host** strategies to enhance anti-cancer benefits.
Each milestone underscored the need for precise immunogenetic matching and potent yet safe **conditioning** regimens. Over time, improvements in infection prophylaxis, supportive care, and laboratory monitoring cemented the procedure’s role in oncology and beyond.
Advances in Conditioning Regimens and Immunotherapy
Conditioning regimens prepare patients for marrow infusion by eradicating malignant clones and suppressing host immunity. Two main approaches dominate clinical practice:
- Myeloablative conditioning: High-dose chemotherapy or total body irradiation, ensuring maximum tumor kill but with increased toxicity.
- Reduced-intensity conditioning: Lower doses to limit organ damage, relying more on donor immune cells for tumor eradication.
Recent innovations have integrated targeted **immunotherapy** alongside standard conditioning:
- Monoclonal antibodies (e.g., anti-CD20, anti-CD52) to deplete malignant and immune cells selectively.
- Checkpoint inhibitors enhancing T-cell response against residual disease.
- CAR-T cell therapy post-transplant to eradicate minimal residual disease and reduce relapse.
These advances aim to balance effective cancer control with reduced transplant-related mortality, expanding eligibility to older or frailer patients.
Donor Selection and Graft Sources
Optimal donor choice remains a cornerstone of successful transplantation. While **matched** sibling donors historically offered the best outcomes, alternative sources have broadened access:
- Matched unrelated donors identified through global registries.
- Haploidentical donors (usually a parent or child), with post-transplant cyclophosphamide to prevent rejection.
- Cord blood units, rich in naïve stem cells and tolerant to HLA mismatches.
- Peripheral blood stem cells, mobilized by cytokine administration and harvested via apheresis.
Each graft source carries unique advantages: cord blood offers rapid availability but slower **engraftment**, whereas peripheral blood yields quicker immune recovery but higher chronic **graft-versus-host** risk. Tailoring choices to disease type, urgency, and patient comorbidity has become a nuanced art backed by evolving data.
Managing Graft-versus-Host Disease and Engraftment
Acute and Chronic GvHD: Challenges and Solutions
Graft-versus-host disease (GvHD) arises when donor immune cells attack host tissues. Acute GvHD typically manifests within 100 days post-transplant, affecting skin, liver, and gut. Chronic GvHD can appear later, with systemic fibrosis and autoimmune-like features. Standard prophylaxis combines calcineurin inhibitors (cyclosporine or tacrolimus) with methotrexate or mycophenolate.
Emerging Therapies and Supportive Care
- Biologic agents targeting cytokines (e.g., anti-IL-6, anti-TNF) to modulate inflammation.
- Mesenchymal stromal cells infused to promote immune tolerance and tissue repair.
- Extracorporeal photopheresis for refractory chronic GvHD, reducing steroid dependence.
Monitoring **engraftment** kinetics through chimerism assays guides immunosuppressive tapering and anticipatory GvHD management, improving long-term outcomes.
Current Trends and Future Directions
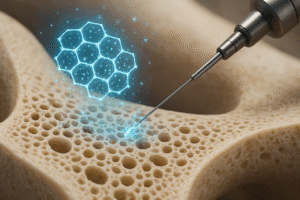
Research frontiers aim to refine the therapeutic index of bone marrow transplantation and extend its curative potential:
- Gene editing technologies (e.g., CRISPR/Cas9) to correct inherited mutations in patient-derived stem cells.
- Ex vivo expansion of cord blood stem cells to accelerate engraftment and broaden graft utility.
- CAR-NK and CAR-macrophage therapies as adjuncts to enhance anti-tumor immunity without escalating GvHD.
- Personalized conditioning guided by pharmacogenomics to optimize drug dosing and minimize toxicity.
Integration of artificial intelligence in donor selection, risk stratification, and post-transplant monitoring promises a new era of precision medicine. As transplant centers worldwide collaborate on large-scale registries and clinical trials, the horizon for curing hematologic diseases will continue to expand, driven by innovation and the unwavering goal of improving patient survival and quality of life.