Maintaining optimal bone integrity is a fundamental aspect of athletic performance and long-term health. Athletes face unique challenges that place their skeletal system under substantial strain, making it critical to adopt evidence-based strategies for risk reduction and structural reinforcement. This article delves into the multifaceted aspects of bone health in athletes, outlining key concerns and effective prevention tactics.
Importance of Bone Health in Athletic Performance
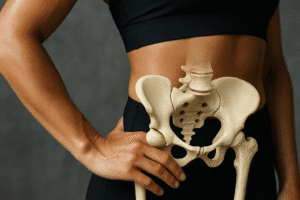
Athletic success is tightly linked to robust skeletal function. Beyond providing a rigid framework, bones serve as a reservoir for minerals and contribute to locomotion through the interplay of muscle forces. Enhanced bone mineral density allows athletes to generate higher power outputs, sustain rigorous training schedules, and reduce downtime due to injury. Conversely, compromised skeletal strength can hamper agility, speed, and stamina, ultimately undermining competitive objectives.
- Structural support: The skeleton withstands impact forces during running and jumping.
- Mineral storage: Bones regulate systemic levels of calcium and phosphorus.
- Molecular signaling: Osteocytes release factors influencing muscle adaptation.
Understanding the physiology of bone remodeling—where osteoblasts form new bone and osteoclasts resorb old matrix—is crucial. Imbalances in this cycle may precipitate early-onset osteopenia or osteoporosis, especially under the high demands of professional training routines.
Identifying Common Skeletal Risks
Athletes are predisposed to specific bone-related injuries and conditions. Recognizing these risks enables preemptive interventions.
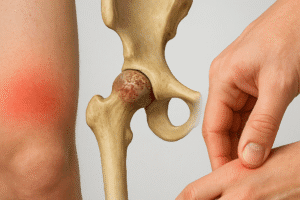
Stress Fractures
- Microscopic cracks from repetitive loading, particularly in weight-bearing bones.
- High incidence in runners, gymnasts, and military recruits.
- Symptoms include localized pain, swelling, and functional impairment.
Delayed diagnosis can lead to full cortical breaks, necessitating extended rest and rehabilitation. Early detection relies on detailed history-taking and targeted imaging.
Relative Energy Deficiency in Sport (RED-S)
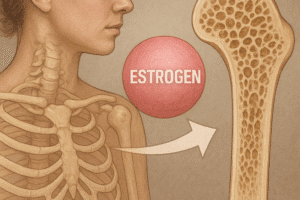
- Inadequate caloric intake relative to expenditure disrupts hormonal homeostasis.
- Leads to reduced energy availability, altered gonadal function, and impaired bone turnover.
- Common among endurance athletes and aesthetic-sport participants.
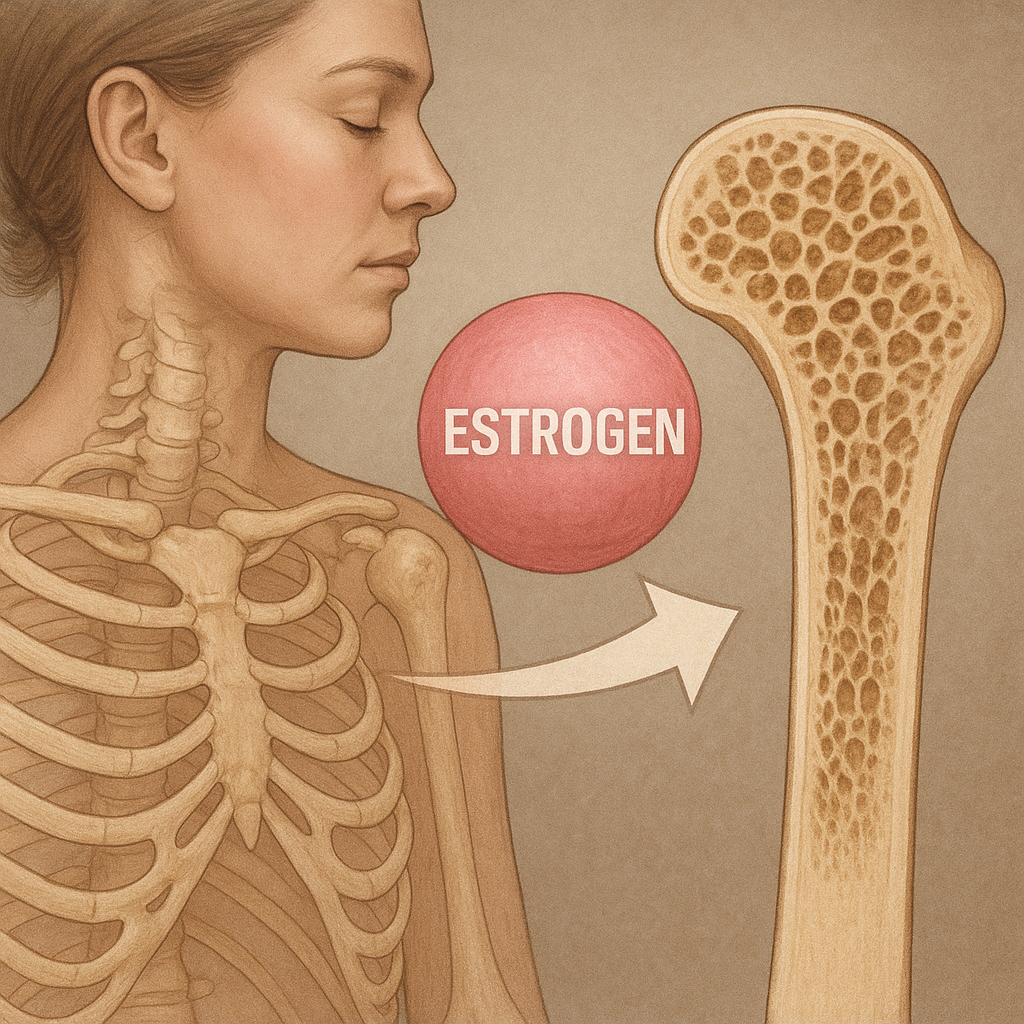
RED-S compromises hormonal balance, diminishing estrogen or testosterone levels and accelerating bone loss. Prevention demands vigilance in dietary monitoring and menstrual or hormonal status assessments.
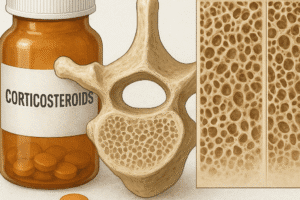
Osteoporosis and Osteopenia in Young Athletes
Though typically associated with older adults, compromised bone mass can emerge in adolescence. Contributing factors include:
- Excessive training without adequate recovery.
- Low body mass index and restrictive dieting.
- Genetic predispositions affecting calcium absorption.
Proactive screening for low bone density in at-risk groups is essential to avert chronic skeletal fragility.
Prevention Strategies for Sustained Bone Strength
Effective prevention integrates nutritional, mechanical, and medical interventions.
Optimizing Nutrition
- Ensure sufficient calcium intake (1,000–1,300 mg daily) through dairy or fortified alternatives.
- Maintain adequate vitamin D levels (20–50 ng/mL) to enhance calcium absorption.
- Include protein sources rich in amino acids to support collagen synthesis.
- Incorporate micronutrients like magnesium and vitamin K for bone matrix formation.
Dietary plans should be individualized, taking into account energy demands, dietary restrictions, and cultural preferences. Collaboration with a sports dietitian ensures balanced macronutrient distribution without risking RED-S.
Strategic Loading and Exercise
- Implement weight-bearing exercises such as hopping drills, plyometrics, and resistance training.
- Periodize training cycles to alternate high-impact weeks with recovery phases.
- Integrate cross-training to diversify loading patterns and mitigate overuse.
Mechanical stimuli provoke osteogenic responses via the mechanotransduction pathways. Gradual progression in intensity and volume reduces the likelihood of stress fractures.
Medical and Monitoring Approaches
- Conduct regular bone density assessments using DXA scans to track changes over time.
- Use blood tests to measure bone turnover markers such as osteocalcin and CTX.
- Employ wearable technology to monitor training load and detect deviations in gait or impact forces.
Timely identification of bone health deviations enables targeted interventions—ranging from dietary adjustments to temporary activity modifications.
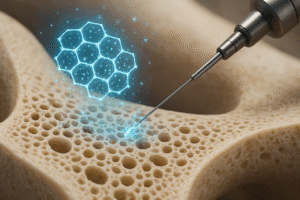
Advanced Diagnostic and Therapeutic Modalities
State-of-the-art imaging and treatment options enhance precision in both detection and management of bone disorders.
- MRI and ultrasound for early visualization of periosteal reactions and stress responses.
- High-resolution peripheral quantitative computed tomography (HR-pQCT) for three-dimensional bone microarchitecture.
- Biophysical therapies like low-intensity pulsed ultrasound (LIPUS) to accelerate fracture healing.
Emerging pharmacological agents—such as sclerostin inhibitors—offer novel pathways to boost bone formation. Integration of these modalities into athlete care protocols demands interdisciplinary coordination among sports physicians, radiologists, and physiotherapists.
Conclusion
Holistic management of bone health in athletes requires a synergy between preventive nutrition, biomechanical conditioning, and sophisticated monitoring. By prioritizing skeletal integrity, athletes can optimize performance, extend their competitive careers, and safeguard long-term well-being.