The quest for restoring skeletal function in patients suffering from traumatic injuries, congenital defects, or degenerative diseases has spurred remarkable advances in the field of bone regeneration. Harnessing the power of biomaterials, scientists seek to develop innovative platforms that support new tissue formation, promote osteogenesis, and integrate seamlessly with the host environment. This article explores the latest developments in composite materials, scaffold fabrication methods, biological enhancements, and emerging clinical applications that are reshaping strategies in regeneration medicine.
Design and Properties of Modern Biomaterials
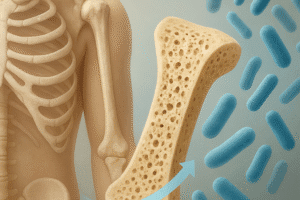
Material selection remains a cornerstone for achieving optimal healing outcomes. An ideal scaffold must exhibit high biocompatibility, mechanical strength matched to native bone, and a degradation profile aligned with tissue ingrowth. Researchers are investigating a diverse palette of substances:
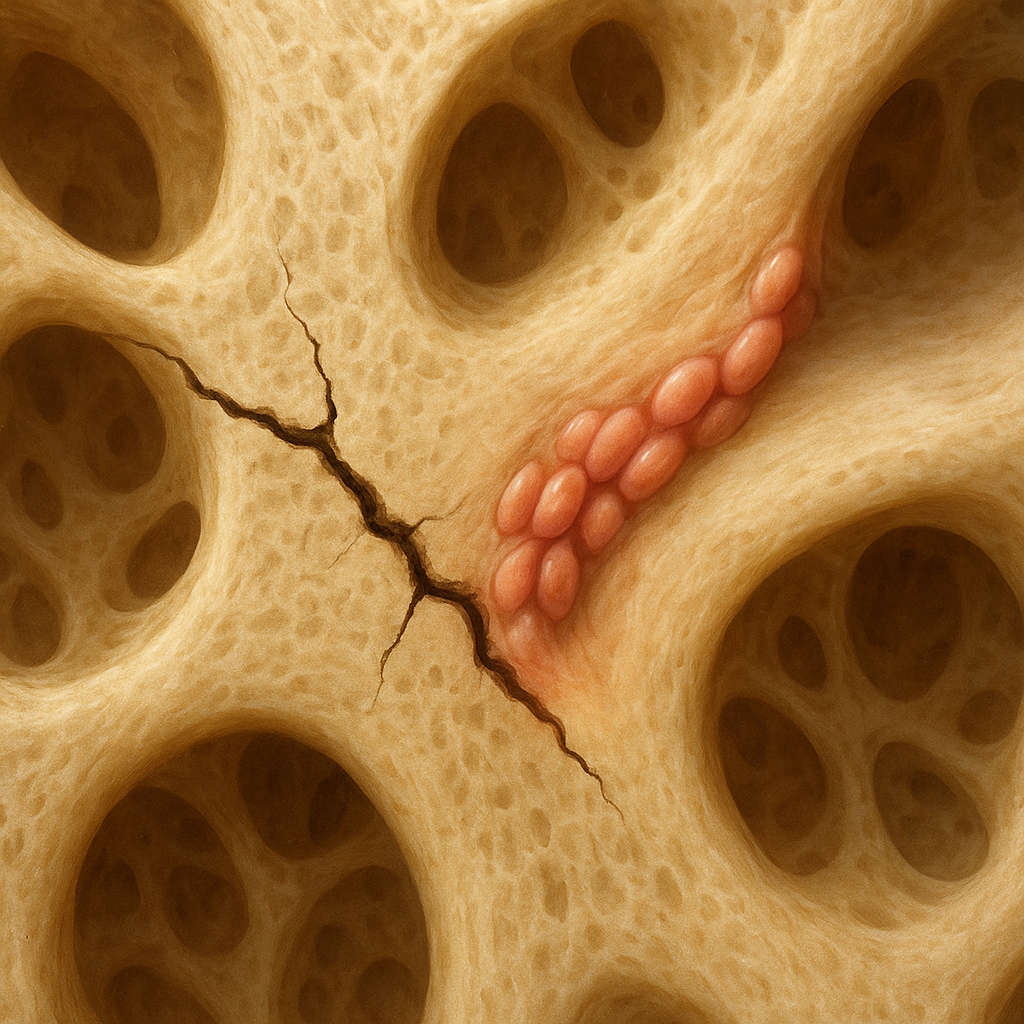
- Calcium phosphates: Predominantly hydroxyapatite and tricalcium phosphate, these ceramics mirror the mineral phase of natural bone, encouraging cellular adhesion and mineral deposition.
- Polymeric matrices: Synthetic polymers such as poly(lactic-co-glycolic acid) (PLGA) and natural biopolymers like collagen or chitosan offer tunable degradation rates and elasticity reminiscent of trabecular bone.
- Composite blends: By combining ceramics with polymers, composites achieve the best of both worlds—rigidity from the inorganic component and toughness from the organic phase.
- Metallic frameworks: Titanium alloys and magnesium-based materials provide superior load-bearing capacity and can be surface-engineered to enhance osseointegration.
Each class of biomaterial demands careful characterization. Mechanical testing (compressive strength, elastic modulus), in vitro cytotoxicity assays, and in vivo animal models collectively guide the selection process. Innovative surface modifications—such as peptide immobilization or plasma treatments—further tailor cell–material interactions, encouraging osteoblast proliferation and vascularization.
Advanced Scaffold Technologies
Scaffolds function as temporary matrices that support cell homing, proliferation, and extracellular matrix deposition. Recent breakthroughs leverage additive manufacturing, microfabrication, and nanotechnology:
- 3D printing: Precise layer-by-layer construction enables patient-specific implants derived from CT or MRI data. Customized architectures optimize pore interconnectivity and mechanical integrity.
- Electrospinning: Produces nanofibrous meshes that mimic the natural collagen network, providing high surface area for cell attachment and growth factor adsorption.
- Bioprinting: Emerging techniques deposit bioinks comprised of living cells and hydrogels, directly generating vascularized tissue constructs with spatial control over cellular placement.
- Microfluidic systems: Microchannel networks simulate fluid perfusion, enhancing nutrient transport and waste removal in large scaffolds to sustain viable cell populations.
Control over scaffold architecture at the micro- and nanoscale has profound effects on mechanotransduction pathways. Aligned fiber orientation can direct cell shape and lineage commitment, while gradient pore sizes support sequential tissue maturation—facilitating both cortical and cancellous bone formation within a single implant.
Biological Enhancements and Growth Factors
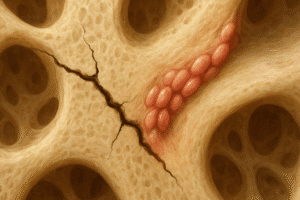
Integrating bioactive molecules represents a potent strategy to accelerate repair. Localized release of growth factors and incorporation of stem cells elevate healing beyond what passive scaffolds can achieve.
- Bone morphogenetic proteins (BMPs): BMP-2 and BMP-7 are FDA-approved cytokines that strongly induce mesenchymal stem cells to differentiate into osteoblasts. Controlled delivery systems—such as heparinized carriers or hydrogel depots—limit supraphysiological bursts and reduce side effects.
- Platelet-derived factors: Platelet-rich plasma (PRP) provides a cocktail of growth-stimulating proteins, including PDGF and TGF-β, promoting angiogenesis and matrix synthesis.
- Stem cell therapies: Multipotent cells from bone marrow, adipose tissue, or induced pluripotent sources offer robust osteogenic potential. Preconditioning with hypoxia or mechanical stimuli further enhances their regenerative capacity.
- Gene delivery: Viral and nonviral vectors can transfect cells within the scaffold, driving sustained production of osteoinductive factors. CRISPR-based approaches to upregulate key transcription factors like RUNX2 are under investigation.
Successful implementation requires a fine balance between scaffold degradation and biofactor release kinetics. Combining inorganic particles embedded with growth factors in polymer matrices affords spatial and temporal control, crucial for orchestrating the complex stages of inflammation, proliferation, and remodeling.
Clinical Applications and Future Directions
Translation from bench to bedside has been bolstered by numerous clinical trials evaluating novel constructs for spinal fusion, long bone defects, and maxillofacial reconstruction. Key considerations include:
- Regulatory compliance: Ensuring materials meet stringent safety and efficacy standards set by agencies like the FDA and EMA.
- Scalability: Manufacturing protocols must support consistent quality at commercial volumes, maintaining batch-to-batch reproducibility.
- Cost-effectiveness: Balancing advanced functionalities with affordability to enhance access and adoption in diverse healthcare settings.
- Long-term outcomes: Monitoring implant integration, mechanical stability, and potential immunogenic responses over extended periods.
Emerging frontiers in the field include smart biomaterials that respond to mechanical cues by releasing additional growth factors, and nanomaterial-enabled sensors that provide real-time feedback on the healing process. Research into immunomodulatory scaffolds aims to harness the body’s innate defense mechanisms, creating a pro-regenerative microenvironment. As multidisciplinary collaborations between materials scientists, biologists, and clinicians continue to flourish, the horizon for scaffolds in bone repair appears brighter than ever.