Research into new treatments for osteoarthritis has accelerated as the global burden of joint degeneration continues to grow. This article explores the underlying mechanisms of the disease, examines current therapeutic limitations, and highlights cutting-edge strategies ranging from advanced pharmacological agents to innovative tissue-engineering techniques. Clinicians and researchers alike are striving to deliver more effective, safe, and personalized treatment options to improve patient quality of life and delay or eliminate the need for joint replacement surgeries.
Pathophysiology and Molecular Insights
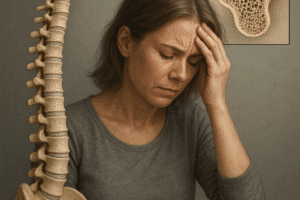
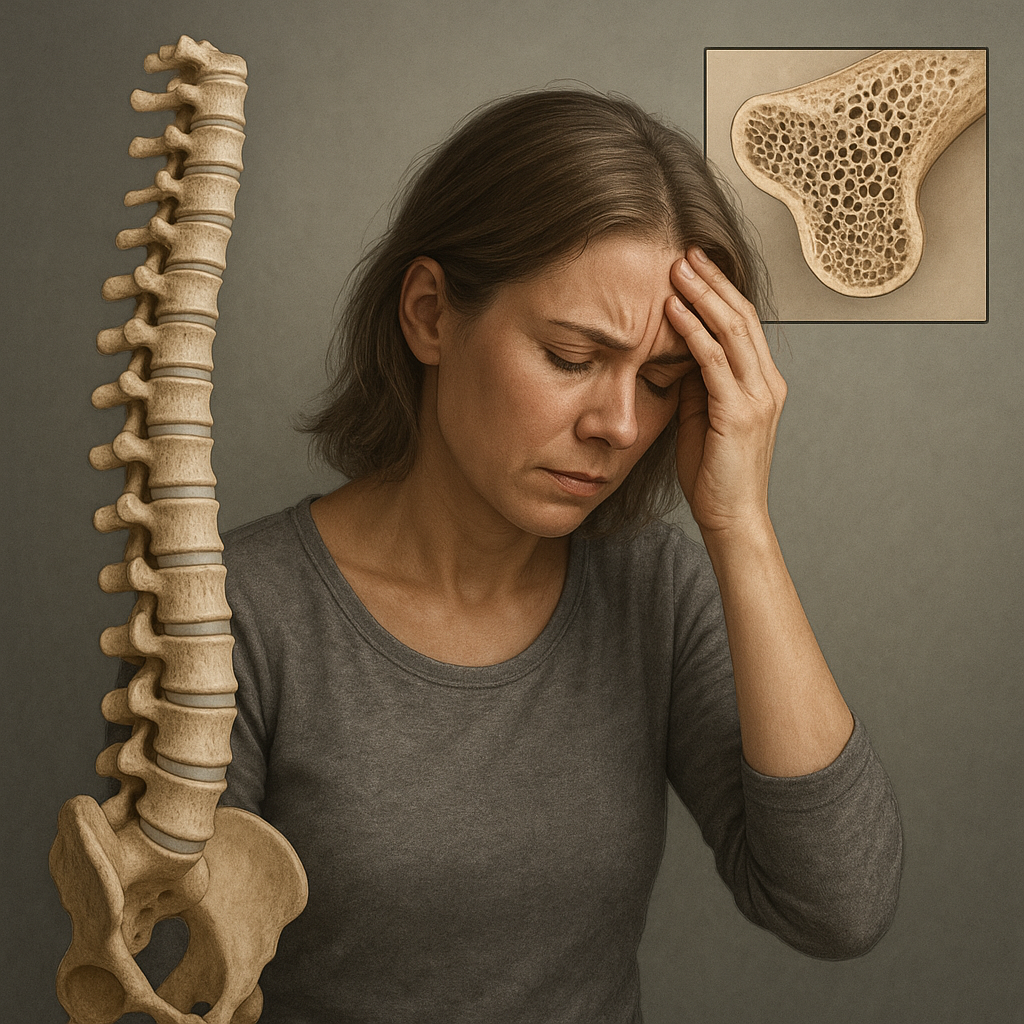
Osteoarthritis is characterized by progressive degradation of articular cartilage, subchondral bone remodeling, and synovial inflammation. Complex interactions among chondrocytes, extracellular matrix components, immune cells, and mechanical stressors drive the disease. Key molecular pathways implicated include:
- Overproduction of matrix metalloproteinases (MMPs) and aggrecanases, leading to cartilage extracellular matrix breakdown.
- Pro-inflammatory cytokines such as interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α) that perpetuate synovitis and pain.
- Alterations in subchondral bone remodeling mediated by osteoclast and osteoblast imbalance, contributing to osteophyte formation and sclerosis.
- Oxidative stress and mitochondrial dysfunction in chondrocytes that accelerate apoptosis and tissue damage.
Recent proteomic and genomic studies have unveiled potential biomarkers for early diagnosis and therapeutic monitoring. Identification of specific microRNAs and cytokine profiles may guide targeted interventions before irreversible joint damage occurs.
Conventional Therapies and Their Limitations
Current standard-of-care focuses on symptom relief and functional improvement rather than disease modification. Common modalities include:
- Analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) for pain management.
- Intra-articular injections of corticosteroids for acute synovitis suppression.
- Viscosupplementation with hyaluronic acid to restore joint lubrication.
- Physical therapy and lifestyle modifications to reduce load on affected joints.
While these approaches can yield temporary relief, they do not arrest structural degeneration. Long-term NSAID use carries gastrointestinal and cardiovascular risks, and repeated steroid injections can accelerate cartilage loss. Joint replacement remains the definitive solution for end-stage disease, but prosthesis lifespan and surgical complications limit its appeal for younger patients.
Novel Pharmacological Treatments
Pharmaceutical research is now targeting molecular drivers of osteoarthritis in an effort to achieve true disease modification. Emerging drug classes include:
- Biologic agents such as monoclonal antibodies against IL-1β and TNF-α, designed to quell chronic inflammation with greater specificity than traditional NSAIDs.
- Small-molecule inhibitors of MMPs and aggrecanases that prevent extracellular matrix degradation.
- Wnt pathway modulators to balance subchondral bone remodeling and inhibit osteophyte formation.
- Synthetic peptides and analogues of growth factors (e.g., transforming growth factor-β, insulin-like growth factor-1) to stimulate chondrocyte anabolism.
Phase II and III clinical trials are underway for several candidates. For example, intra-articular delivery of a novel anti-nerve growth factor (NGF) antibody has shown promising reductions in pain intensity and improved joint function. Pharmacokinetic optimization aims to achieve sustained local drug concentrations while minimizing systemic exposure and adverse effects.
Regenerative Medicine Approaches
Advances in regenerative medicine offer exciting possibilities for repairing or replacing damaged joint tissues. Key strategies include:
Cell-Based Therapies
Mesenchymal stem cells (MSCs), isolated from bone marrow, adipose tissue, or synovium, possess the capacity to differentiate into chondrocytes and secrete trophic factors that modulate inflammation and promote tissue repair. Ongoing studies investigate:
- Autologous versus allogeneic MSC transplantation to determine optimal cell sourcing and immune compatibility.
- Preconditioning MSCs with hypoxia or growth factors to enhance their reparative potency.
- Engineered scaffolds seeded with MSCs to provide structural support and spatial organization for new cartilage formation.
Gene and Exosome Therapies
Gene delivery systems are being developed to achieve targeted expression of therapeutic proteins directly within the joint environment. Techniques under exploration include:
- Viral vectors encoding anti-inflammatory cytokines or cartilage anabolic factors.
- Non-viral nanoparticles for locally controlled release of genetic material.
- MSC-derived exosomes carrying microRNAs that downregulate catabolic gene expression and stimulate chondrocyte survival.
Preclinical models have demonstrated that these approaches can restore cartilage integrity and reduce joint inflammation without the risks associated with systemic immunosuppression.
Innovations in Drug Delivery and Imaging
Targeted delivery systems aim to maximize drug concentrations at the disease site while reducing systemic toxicity. Recent advancements include:
- Hydrogel-based carriers that release therapeutic agents in response to changes in pH or enzymatic activity within the osteoarthritic joint.
- Nanoformulations that enhance penetration into cartilage matrix and prolong intra-articular drug retention.
- Ultrasound-responsive microbubbles that enable on-demand, externally triggered release of encapsulated drugs.
Parallel progress in high-resolution imaging modalities, such as quantitative MRI and novel PET tracers, allows clinicians to visualize early cartilage lesions and monitor treatment efficacy at a molecular level.
Future Perspectives and Challenges
Although many promising therapies are nearing clinical application, several hurdles remain:
- Standardization of outcome measures and biomarkers to compare results across trials.
- Cost-effectiveness evaluations to ensure accessibility of advanced treatments.
- Optimization of dosing regimens and delivery routes for durable efficacy.
- Long-term safety assessments, particularly for gene and cell-based interventions.
Integration of artificial intelligence and machine learning in patient stratification could usher in an era of truly personalized treatment for osteoarthritis. By combining genetic, imaging, and clinical data, algorithms may predict which individuals will respond best to specific therapies. Collaborative efforts among researchers, clinicians, and industry stakeholders will be essential to translate these innovations into routine orthopedic care.