Stem cell therapy has emerged as a revolutionary approach in orthopedics, offering promising avenues to enhance the natural process of bone repair. By harnessing the unique properties of mesenchymal stem cells and optimizing the design of bioactive scaffolds, researchers aim to accelerate osteogenesis and restore skeletal integrity. This article explores fundamental mechanisms, clinical experiences, and future trends that define the interface between regenerative medicine and bone healing.
The Biology of Bone Regeneration
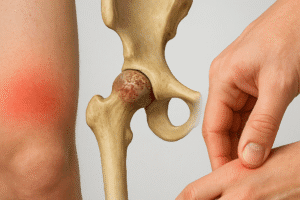
Understanding the intrinsic capacity of bone to heal is essential before discussing advanced interventions. Fracture repair follows a finely orchestrated sequence involving inflammation, repair, and remodeling phases. During inflammation, damaged cells release cytokines and growth factors that recruit progenitor cells. The subsequent repair stage relies on endochondral ossification, where cartilage is gradually replaced by bone, while direct intramembranous ossification contributes to cortical continuity. Finally, remodeling produces mature lamellar bone adapted to mechanical demands.
Cellular Players and Signaling Pathways
- Osteoblasts: Derived from mesenchymal progenitors, these cells deposit collagen matrix and mineralize new bone.
- Osteoclasts: Responsible for bone resorption, they ensure removal of damaged tissue and shape remodeling.
- Endothelial cells: Facilitate angiogenesis, supplying oxygen and nutrients critical for bone repair.
- Inflammatory cells: Neutrophils and macrophages secrete factors like VEGF and TGF-β to modulate healing.
Key molecular pathways include BMP (Bone Morphogenetic Protein), Wnt/β-catenin, and Notch signaling. These cascades regulate cell fate decisions, differentiation, and matrix production. Dysregulation may result in delayed union or non-union fractures, motivating techniques to reinforce the natural regenerative machinery.
Stem Cell Types and Their Role in Healing
A range of stem cell populations have been investigated for bone therapy. The most extensively studied are mesenchymal stem cells (MSCs) derived from bone marrow, adipose tissue, and umbilical cord. Their potential lies in multilineage differentiation, immunomodulatory effects, and secretion of trophic factors.
Bone Marrow–Derived MSCs
Bone marrow aspirate contains a small fraction of MSCs capable of differentiating into osteoblasts under osteoinductive conditions. Ex vivo expansion enables delivery of therapeutically relevant cell numbers. Clinical trials report enhanced callus formation and improved biomechanical strength in long-bone defects when MSCs are implanted with appropriate carriers.
Adipose-Derived Stem Cells
Adipose tissue offers a readily accessible and abundant source of MSC-like cells. Despite a slightly lower osteogenic potential compared to bone marrow MSCs, these cells demonstrate potent paracrine actions and can be harvested via minimally invasive liposuction. Their incorporation into biomaterials has shown accelerated healing in preclinical models.
Pluripotent Stem Cells
Embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) present unlimited expansion capacity and robust differentiation potential. Safety concerns regarding teratoma formation and immunogenicity have driven research into lineage-committed progenitors or pre-differentiated osteoprogenitors from these sources.
Clinical Applications and Challenges
Translating laboratory success into routine patient care necessitates careful consideration of delivery methods, regulatory guidelines, and cost-effectiveness. Several strategies are currently under investigation:
- Direct injection of cell suspensions into non-union fracture sites
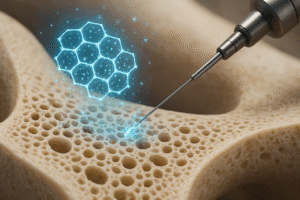
- Seeding of cells onto porous scaffolds loaded with growth factors
- Fabrication of cell-laden hydrogels for minimally invasive implantation
Scaffold-Based Therapies
Composite scaffolds combining ceramics (e.g., hydroxyapatite), polymers (e.g., PLGA), and bioactive molecules provide a three-dimensional framework supporting cell attachment, proliferation, and matrix deposition. The scaffold’s architecture and degradation kinetics are engineered to match new tissue formation while allowing vascular ingrowth.
Immunomodulation and Allogeneic Transplants
Allogeneic MSCs offer an off-the-shelf solution, but immune rejection remains a hurdle. However, MSCs exert immunomodulation by secreting anti-inflammatory cytokines and evading host detection. Clinical studies have demonstrated safety and preliminary efficacy of allogeneic cell products in treating osteonecrosis and critical-size bone defects.
Regulatory and Ethical Considerations
- Good Manufacturing Practice (GMP) standards for cell processing
- Long-term follow-up to monitor potential tumorigenicity
- Ethical sourcing of human tissues, particularly for ESCs
Manufacturers must navigate strict regulatory pathways to ensure product consistency, sterility, and potency. The cost of cell therapies and reimbursement policies also impact widespread adoption.
Future Directions in Bone Regenerative Medicine
The next generation of therapies will likely integrate advanced biomaterials, genetic engineering, and real-time monitoring technologies. Innovations include:
- 3D bioprinting of patient-specific bone grafts combining cells and biodegradable polymers
- Gene-editing techniques (CRISPR/Cas9) to enhance MSC osteogenic potential
- Smart scaffolds that release growth factors in response to mechanical stimuli
- Non-invasive imaging modalities to track cell survival and matrix formation
Personalized Approaches
Leveraging genomic profiling and biomechanical analysis, personalized bone regeneration protocols can be designed to accommodate individual healing capacities and defect characteristics. Such precision medicine approaches promise to maximize therapeutic outcomes while minimizing risks.
Integration with Digital Health
Wearable sensors and telemedicine platforms could enable continuous monitoring of fracture healing, guiding timely interventions and optimizing rehabilitation regimens. Data analytics and machine learning may predict healing trajectories based on patient-specific factors.
As our understanding of the cellular and molecular drivers of bone repair deepens, stem cell–based therapies will become increasingly sophisticated. Combining transplantation techniques, engineered biomaterials, and real-time diagnostics paves the way for durable skeletal regeneration even in the most challenging clinical scenarios.