Bone remodeling represents a continuous process of renewal that maintains **homeostasis** and structural integrity of the adult skeleton. This dynamic cycle involves coordinated actions of specialized cells and signaling pathways that detect and repair microdamage, adapt bone architecture to mechanical loads, and regulate mineral balance. A deeper understanding of cellular mechanisms and external influences is crucial for developing effective strategies to prevent and treat skeletal disorders such as osteoporosis, osteoarthritis, and fracture nonunions.
Cellular and Molecular Mechanisms of Bone Remodeling
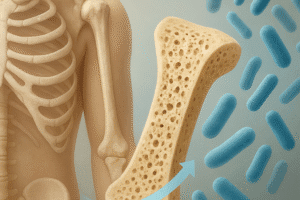
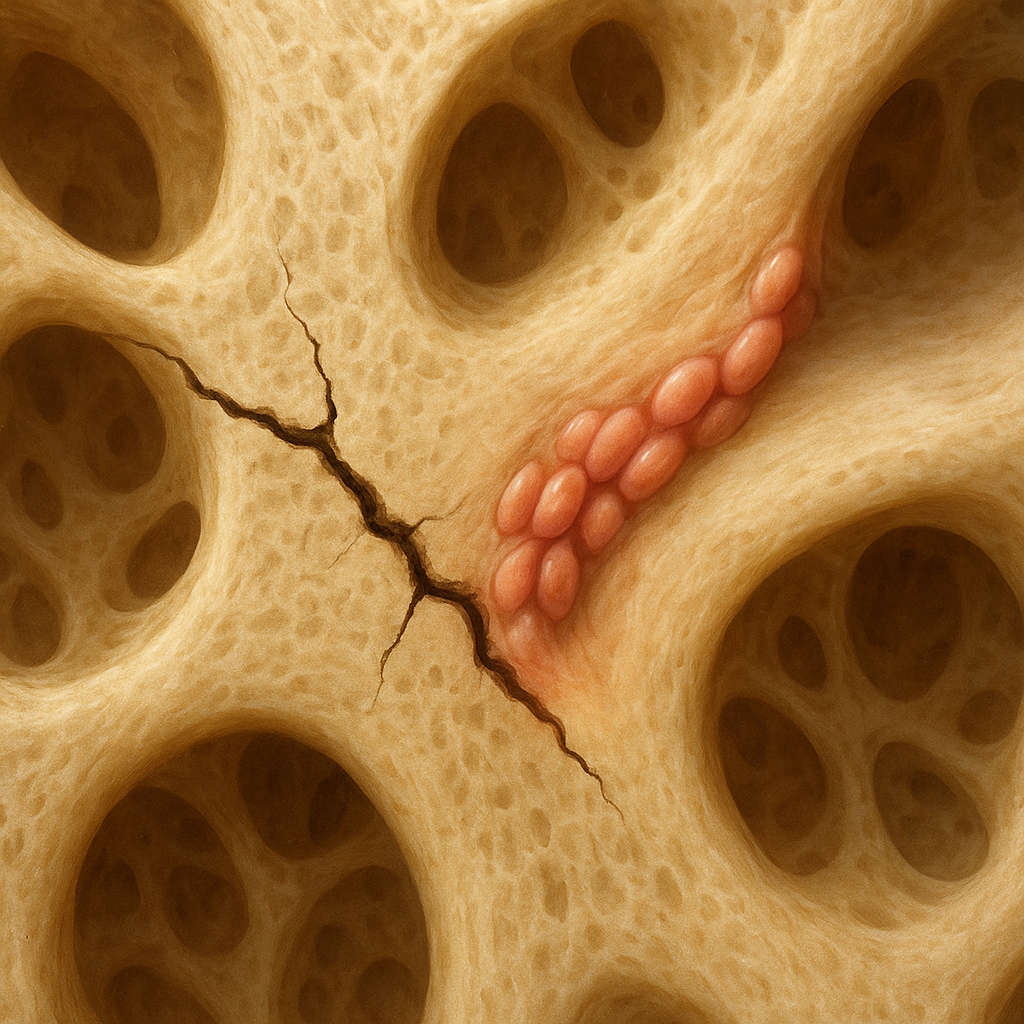
The bone remodeling cycle comprises two main phases: bone resorption and bone formation. During resorption, multinucleated osteoclasts adhere to the bone surface, creating an acidic microenvironment that dissolves mineral components and degrades the organic scaffold. This phase is tightly balanced by the activity of mononuclear osteoblasts, which subsequently populate excavated sites and deposit new matrix.
Role of Osteoclasts and Osteoblasts
- Osteoclasts differentiate from hematopoietic precursors under the control of RANKL (receptor activator of nuclear factor κB ligand) and M-CSF (macrophage colony-stimulating factor).
- Osteoblasts originate from mesenchymal stem cells, synthesizing collagen type I and non-collagenous proteins that constitute the extracellular matrix.
- Coupling factors such as IGF-1 and TGF-β released during resorption stimulate osteoblast recruitment and activation.
Regulatory Signaling Pathways
A network of endocrine and paracrine signals orchestrates remodeling. Key players include:
- Vitamin D: Promotes calcium absorption in the gut and modulates osteoblast function.
- PTH (parathyroid hormone): Intermittent exposure exerts anabolic effects on bone, while continuous elevation favors resorption.
- Cytokines such as IL-1, IL-6 and TNF-α influence osteoclast differentiation and activity.
- Wnt/β-catenin signaling: Essential for osteoblast proliferation and survival, inhibited by sclerostin.
Influences on Bone Remodeling Dynamics
Bone remodeling adapts to both systemic and local stimuli. Mechanical forces, nutritional status, hormonal milieu, and inflammatory conditions each modulate the balance between resorption and formation.
Mechanotransduction and Physical Activity
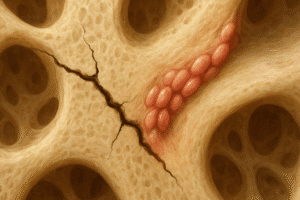
Mechanical loading generates fluid flow within the lacuno-canalicular system, sensed by osteocytes that regulate remodeling through sclerostin and nitric oxide. Adequate weight-bearing exercise enhances bone mass, whereas immobilization leads to accelerated resorption. The concept of microdamage accumulation and targeted remodeling ensures removal of compromised tissue and preservation of mechanical competence.
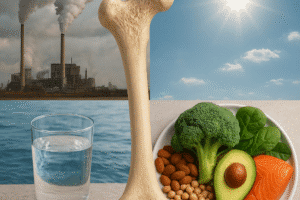
Nutritional and Metabolic Factors
- Calcium and vitamin D are fundamental for mineralization; deficiency triggers secondary hyperparathyroidism.
- Protein intake supplies amino acids for collagen synthesis.
- Micronutrients such as magnesium, phosphorus, and vitamin K support matrix maturation and mineral deposition.
- Endocrine disorders (e.g., hyperthyroidism, hypogonadism) disrupt remodeling rates and compromise bone quality.
Inflammation and Pathological Conditions
Chronic inflammation elevates pro-resorptive mediators, leading to net bone loss seen in rheumatoid arthritis and other autoimmune diseases. Elevated levels of TNF-α and IL-17 stimulate osteoclasts and impede osteoblast differentiation, creating an imbalance that favors catabolic activity. In contrast, localized bone remodeling associated with fracture healing utilizes a similar cascade of signals but in a spatially restricted manner to regenerate tissue.
Clinical Considerations and Therapeutic Strategies
Translating insights into bone remodeling into clinical practice has led to a range of interventions aimed at restoring skeletal health. Treatment modalities address both increased resorption and impaired formation.
Antiresorptive Therapies
- Bisphosphonates: Inhibit farnesyl pyrophosphate synthase in osteoclasts, reducing resorption and fracture risk.
- Denosumab: A monoclonal antibody against RANKL that decreases osteoclastogenesis.
- Selective estrogen receptor modulators (SERMs): Provide estrogen-like benefits on bone with fewer systemic risks.
Anabolic Agents
- PTH analogs (teriparatide): Stimulate osteoblast activity when administered intermittently.
- Romosozumab: A sclerostin inhibitor that both increases formation and decreases resorption.
- Investigational therapies targeting Wnt agonists or TGF-β modulators aim to further enhance bone mass.
Adjunctive and Lifestyle Interventions
Optimal management includes:
- Dietary counseling to ensure adequate intake of calcium, vitamin D, and protein.
- Structured exercise programs emphasizing resistance and balance to stimulate mechanotransduction and prevent falls.
- Monitoring and correction of endocrine imbalances.
- Smoking cessation and moderation of alcohol intake to reduce oxidative stress and inflammatory insults to bone tissue.
Emerging research explores the potential of cell-based therapies, microRNA modulation, and biomaterial scaffolds to promote targeted regeneration in localized bone defects. Understanding the interplay between systemic factors and local microenvironments remains critical for advancing personalized treatment strategies that preserve skeletal integrity and function.