Orthopedic implant technologies have undergone remarkable transformations over the past decades, reshaping approaches to bone repair, joint replacement, and trauma management. By leveraging breakthroughs in materials, engineering, and biological sciences, modern implants provide enhanced functionality, longer lifespans, and improved patient outcomes. This article explores key innovations, from novel biomaterials to advanced manufacturing methods, and considers future directions in the dynamic interplay of bone and medicine.
Background and Clinical Challenges
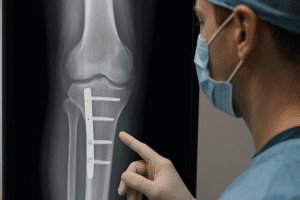
The primary goals of any orthopedic implant include restoring mobility, reducing pain, and ensuring long-term stability. Traditional implants, however, have faced hurdles such as wear-induced debris, aseptic loosening, and infection risks. Surgeons must balance mechanical demands with biological compatibility while considering factors like patient age, activity level, and bone quality.
- Wear and debris generation leading to osteolysis
- Corrosion and metal ion release
- Poor integration with host bone
- Risk of post-operative infection
- Limited lifespan requiring revision surgeries
Overcoming these challenges necessitates a multi-disciplinary approach centered on materials science, biomechanics, and bioengineering principles.
Advanced Materials in Orthopedic Implants
Ceramics and Polymers
Ceramic components, such as alumina and zirconia, offer exceptional hardness, wear resistance, and chemical inertness. Their low friction coefficients make them ideal for joint articulations, minimizing particle generation. Medical-grade polymers like ultra-high-molecular-weight polyethylene (UHMWPE) have also evolved through crosslinking and antioxidant stabilization to resist wear and oxidative degradation.
- Enhanced biocompatibility reduces inflammatory response
- Improved fatigue resistance in cyclic loading
- Advanced polymer blends for shock absorption
Metals and Alloys
Titanium and its alloys remain the gold standard for load-bearing implants due to their favorable strength-to-weight ratio and corrosion resistance. Recent efforts focus on surface texturing and coating to boost osseointegration. Novel alloys incorporating tantalum or niobium demonstrate lower elastic moduli, closely matching cortical bone to mitigate stress shielding.
- Porous metallic scaffolds promoting bone ingrowth
- Bioactive coatings with calcium phosphate layers
- Alloy design for tailored biomechanics
Composite Materials
Combining ceramics, polymers, and metals into composites merges the strengths of each class. For instance, carbon-fiber-reinforced polymers provide customizable stiffness, while bioactive glass-coated polymers encourage mineralization. These hybrid systems can be engineered to degrade gradually, making way for natural bone regeneration.
Technological Innovations and Manufacturing Techniques
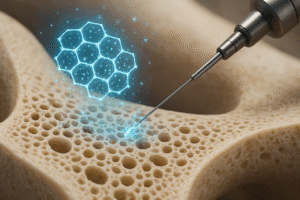
3D Printing and Additive Manufacturing
Additive manufacturing has unlocked possibilities for creating highly complex, patient-specific geometries. Through selective laser melting (SLM) or electron-beam melting (EBM), porous lattice structures mimic trabecular bone, enhancing mechanical interlocking and vascularization. Custom implants designed from CT or MRI data ensure anatomic conformity, reducing surgical time and improving outcomes.
- Tailored pore size for nutrient flow and cell migration
- Reduced material waste and production timelines
- Integration with surgical navigation systems
Surface Modification and Coatings
Surface engineering techniques such as plasma spraying, anodization, and laser texturing refine implant interfaces. Antimicrobial coatings incorporating silver nanoparticles or antibiotic-loaded polymers combat infection. Additionally, biomimetic peptides and growth factors immobilized on surfaces stimulate local bone formation.
- Controlled release of therapeutic agents
- Nanostructured surfaces enhancing cell adhesion
- Reduction of bacterial colonization on implant sites
Smart and Responsive Implants
Emerging smart implants integrate sensors, electronics, and actuators to monitor healing and mechanical loads in real time. Wireless telemetry can track parameters such as pH, temperature, and strain, allowing clinicians to tailor rehabilitation protocols. Shape memory alloys embedded within implants adjust stiffness dynamically, responding to physiological conditions.
Future Directions and Emerging Trends
Looking ahead, the convergence of nanotechnology, regenerative medicine, and digital health promises to redefine implant paradigms. Nanofibrous scaffolds loaded with stem cells or exosomes may accelerate bone regeneration. Gene-activated matrices can deliver osteogenic instructions directly to resident cells. Meanwhile, machine learning algorithms analyzing patient data can predict implant performance and personalize material selection.
- Development of bioresorbable devices for temporary fixation
- Integration of 4D printing for time-dependent shape changes
- Implementation of augmented reality in surgical planning
- Expansion of telemedicine-enabled post-operative monitoring
As orthopedic implants evolve, collaboration among surgeons, engineers, and biologists remains essential. The pursuit of devices that seamlessly integrate with the human body and adapt to its dynamic environment drives ongoing research and clinical trials. Ultimately, these innovations aim to restore mobility, reduce revision rates, and enhance quality of life for patients worldwide.