Vitamin D has emerged as an indispensable factor in maintaining bone integrity and overall skeletal function. Beyond its classical role in calcium homeostasis, this micronutrient exerts effects on the cellular machinery that governs bone formation and resorption. In this article, we will delve into the multifaceted pathways through which vitamin D influences bone health, evaluate the consequences of deficiency, and discuss contemporary strategies for supplementation and therapeutic intervention.
Synthesis, Metabolism, and Mechanisms of Action
Vitamin D exists in two principal forms: cholecalciferol (D3) synthesized in the skin upon ultraviolet B exposure, and ergocalciferol (D2) obtained from certain plant sources. Once ingested or produced cutaneously, it undergoes two hydroxylation steps: first in the liver to form 25-hydroxyvitamin D, and then in the kidney to generate the biologically active 1,25-dihydroxyvitamin D. The latter binds to the vitamin D receptor (VDR), a nuclear receptor that modulates gene transcription in numerous target cells, including osteoblasts, osteoclasts, and intestinal enterocytes.
Within bone tissue, the VDR–ligand complex influences the expression of genes responsible for:
- Intestinal absorption of calcium and phosphate
- Osteoblastic differentiation and matrix mineralization
- Regulation of osteoclastogenesis through RANKL/OPG balance
By orchestrating these pathways, vitamin D ensures optimal skeletal metabolism and resilience against mechanical stress.
Impact on Bone Remodeling Dynamics
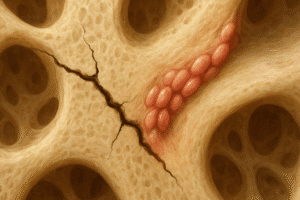
Bone remodeling is a continuous process wherein old or damaged bone is removed by osteoclasts and replaced by new bone formed by osteoblasts. Vitamin D influences both arms of this process:
- Promotion of osteoblastic activity: 1,25-dihydroxyvitamin D stimulates osteoblasts to produce osteocalcin and alkaline phosphatase, proteins essential for collagen synthesis and mineral deposition.
- Modulation of osteoclastic differentiation: Through upregulation of RANKL expression on osteoblasts, vitamin D indirectly fosters osteoclast formation. However, adequate calcium levels—maintained by vitamin D—limit excessive resorption.
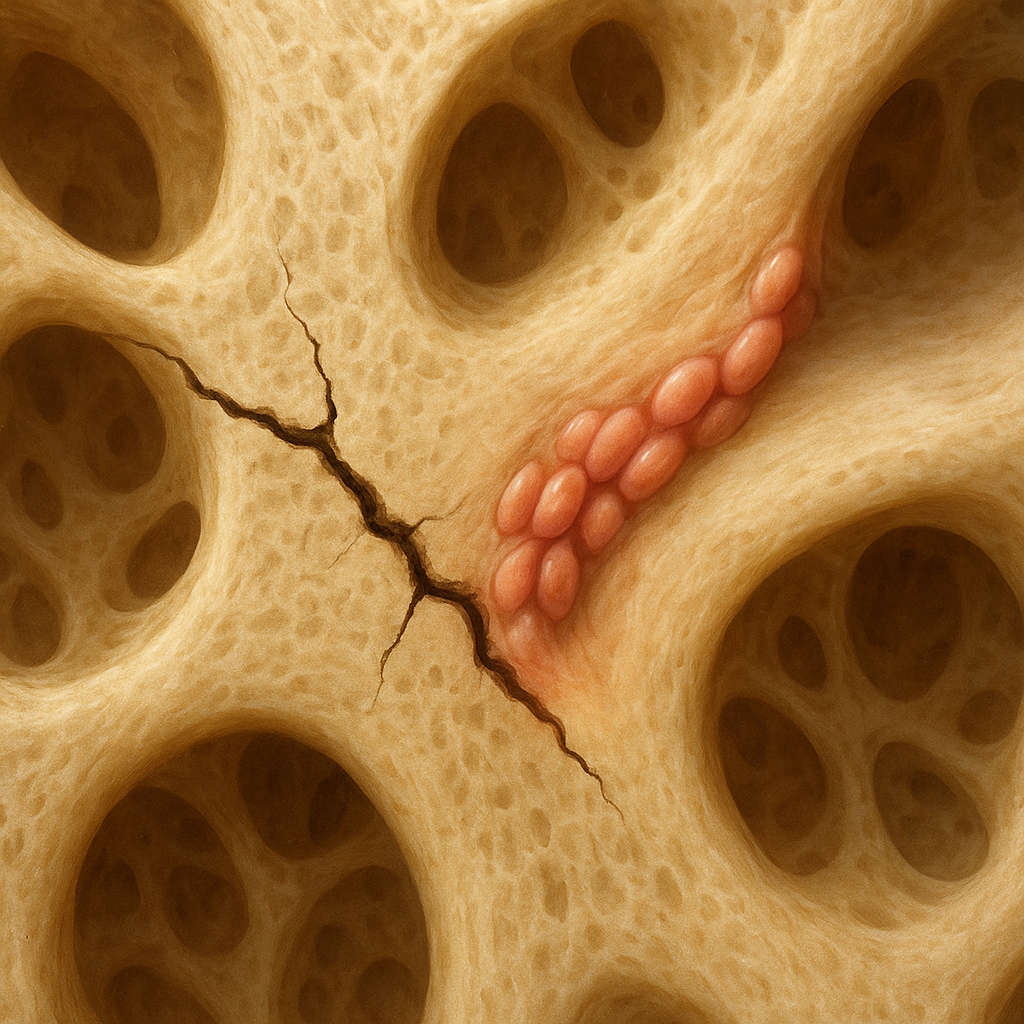
When vitamin D status is optimal, bone turnover remains balanced, preserving structural integrity and density. Conversely, deficiency disrupts this equilibrium, predisposing to microarchitectural deterioration and increased fracture risk.
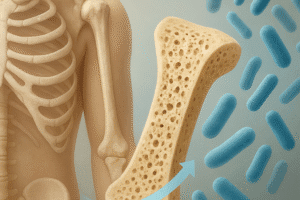
Consequences of Inadequacy and Deficiency
Insufficient vitamin D can result from inadequate sun exposure, poor dietary intake, malabsorption syndromes, or renal impairment. The skeletal manifestations include:
- Rickets in children: characterized by growth plate widening, bone deformities, and delayed mineralization.
- Osteomalacia in adults: marked by bone pain, muscle weakness, and pseudofractures.
- Exacerbation of osteoporosis: accelerated loss of bone mass and heightened susceptibility to low-trauma fractures.
At the molecular level, deficiency impairs intestinal calcium uptake, triggering secondary hyperparathyroidism. Elevated parathyroid hormone levels accelerate bone resorption, further compounding mineral loss. Early recognition of subclinical insufficiency is critical to avert irreversible skeletal damage.
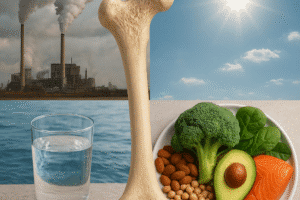
Dietary Sources and Supplementation Strategies
While endogenous synthesis is the primary source of vitamin D for many, dietary intake and supplements play key roles, especially in regions with limited sunlight. Rich food sources include:
- Fatty fish (e.g., salmon, mackerel, sardines)
- Fortified dairy products and plant-based milk alternatives
- Egg yolks and cod liver oil
Supplementation guidelines vary by age, baseline serum 25-hydroxyvitamin D levels, and comorbid conditions. Common regimens include:
- Daily low-dose supplementation (800–2,000 IU of vitamin D3).
- High-dose intermittent dosing (e.g., 50,000 IU weekly for 6–8 weeks) for repletion.
- Combination therapies incorporating calcium to optimize absorption and support bone mineralization.
Monitoring serum 25-hydroxyvitamin D concentrations is essential to tailor therapy and avoid potential toxicity, such as hypercalcemia and soft tissue calcification.
Clinical Trials and Emerging Therapeutics
Recent randomized controlled trials have investigated vitamin D’s role beyond skeletal outcomes, exploring its impact on muscle function, immune modulation, and chronic disease prevention. In bone-specific studies, supplementation has consistently shown benefits in reducing fracture incidence among at-risk elderly populations, particularly when combined with adequate calcium.
Novel Delivery Systems
Advances in pharmaceutics have led to the development of sustained-release formulations and lipid-based carriers, enhancing bioavailability. Nanoparticle encapsulation and transdermal patches are under investigation to improve patient adherence and maintain steady serum levels.
Genetic Considerations
Polymorphisms within the VDR gene influence individual responsiveness to vitamin D. Personalized approaches, incorporating genotyping, may soon allow clinicians to optimize dosing regimens and predict therapeutic outcomes.
Conclusion of Key Insights
Vitamin D’s central role in regulating calcium homeostasis and bone remodeling underscores its significance in preventive and therapeutic bone medicine. Ensuring adequate vitamin D status through sensible sun exposure, dietary sources, and evidence-based supplementation fosters optimal bone density, reduces fracture risk, and supports musculoskeletal health across the lifespan.